Site sections
Editor's Choice:
- Exhibition of autumn crafts "Amazing near" in kindergarten
- Technology and step-by-step instructions for nail gel: steps, rules, process
- White spots on the nails, reasons for what to do, white spots on the nails and folk signs
- Available methods for rapidly increasing blood leukocytes
- Nail and skin fungus will not resist the coffee grounds
- Crocus furniture exhibition. Furniture exhibitions
- Owl tattoo on arm value
- The biggest members in the world
- Fractures of the phalanges of the foot photo
- What is “bad” and “good” cholesterol
Advertising
| Inflammatory diseases |
|
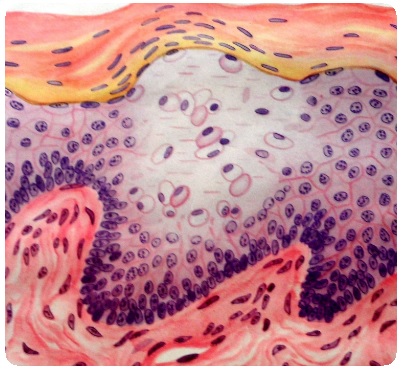
Inflammation is a typical pathological process formed in evolution as a protective and adaptive response of the body to the effects of pathogenic (phlogogenic) factors, aimed at localizing, destroying and removing the phlogogenic agent, as well as eliminating the consequences of its action and is characterized by alteration, exudation and proliferation. Etiology of inflammation: Inflammation occurs as a reaction of the body to the pathogenic stimulus and the damage it causes. Pathogenic, called in this case phlogogenic, stimuli, i.e. causes of inflammation can be diverse: biological, physical, chemical, both exogenous and endogenous. Etiogenic factors: Thrombus, embolus, salt deposition, hemorrhage, tumor Exogenous factors: mechanical, physical, chemical, biological. The main role - the reflex mechanism. Classification: There are three main forms of inflammation: 1) interstitial diffuse; 2) granulomatous; 3) inflammatory hyperplastic (hyperregenerative) growths. When systematizing the types of inflammation, along with clinical and anatomical features take into account: 1) time characteristic of the process (acute and chronic); 2) morphofunctional features of inflammation; 3) pathogenetic specificity of inflammation (immune inflammation). The process is considered acute if it lasts up to 4-6 weeks, but in most cases it ends within 1.5-2 weeks. Depending on the nature of the dominant local process (alteration, exudation or proliferation) there are three types of B. In the case of the prevalence of alterative processes, dystrophy, necrosis develops alterative (necrotic) inflammation. It is observed most often in parenchymal organs in infectious diseases that occur with severe intoxication. There are also exudative and proliferative types V. in accordance with the severity of a process. Exudative V. is characterized by a marked impairment of blood circulation with symptoms of exudation and emigration of leukocytes. By the nature of the exudatedistinguish serous, purulent, hemorrhagic, fibrinous, mixed B. In addition, with the development of B. mucous membranes, when mucus is mixed with the exudate, mucus is referred to as catarrhal B., which is usually combined with exudative B. other types (serous catarrhal, purulent catarrhal, etc.). Proliferative and productive V. is characterized by the dominant reproduction of cells of hematogenous and histogenic origin. Cell infiltrates arise in zone V., which, depending on the nature of the accumulated cells, are round-cell (lymphocytes, histiocytes), plasma-cell, eosinophilic-cell, epithelioid-cell, macrophage infiltrates. IMPORTANCE OF INFLAMMATION FOR THE ORGANISM As with other typical processes, the harmful and useful is combined in an inseparable connection. It combines the mobilization of the body's defenses, and the phenomenon of damage, “breakdown”. The body is protected from the effects of factors alien and harmful to it by delimiting the inflammatory focus from the whole organism, forming a kind of barrier with one-sided permeability around the focus B. Localization of the outbreak B. prevents the spread of infection. Due to the exudation, the concentration of toxic substances in the hearth B is reduced. The inflamed area not only fixes, but also absorbs toxic substances and provides their detoxification. In the outbreak of V. are also created unfavorable conditions for life m / o. The second opposite is that V., being an evolutionarily developed protective process, at the same time has a damaging effect on the organism, always carries within itself an element of destruction. The fight against the “aggressor” in zone B. is inevitably combined with the death of its own cells. In some cases, the alteration begins to predominate, which leads to the death of a tissue or an entire organ. Exudation can cause malnutrition of the tissue, its enzymatic melting, hypoxia and general intoxication. To inflammatory diseases of the maxillofacial region, and in particular, severe forms of odontogenic inflammatory processes are periodontitis, periostitis, osteomyelitis of the jaws and cellulitis of the surrounding soft tissues. Features of the occurrence and course of inflammatory reactions in tissues oral cavity: Granulomatous inflammation characterized by a limited focus of productive, productive-exudative inflammation, the formation of delimited infiltrates is characteristic of inflammatory processes in the maxillofacial region. At the heart of this inflammation are the primary growths of granulation tissue infiltrated with polynuclears, lymphocytes, plasma cells in various ratios. An example of such inflammation is a tooth granuloma, a tumor-like mass near the apex of a tooth made of granulation tissue, surrounded by a fibrous capsule, resulting from chronic inflammation at infection of perodont from the canal of tooth. In cases of development of inflammatory processes in the maxillofacial region, it is necessary to remember the peculiarities of the venous system. The absence of a valvular system in the veins of the face causes the possibility of rapid migration of a blood clot in the upward direction and the occurrence of cortical sinus thrombosis with an extremely life-threatening prognosis. Local and general manifestations of inflammation, the mechanisms of their development. Characteristic of the notion “acute phase response”, acute phase proteins, their clinical significance. LOCAL SYMPTOMS Local reaction in case of acute purulent infection, symptoms manifest themselves in the development of the inflammatory response: ruber (redness), calor (local heat) tumor (swelling), dolor (pain), functio laesa (dysfunction). Redness easily determined upon inspection. It reflects the expansion of blood vessels (arterioles, venules and capillaries), then the blood flow slows down to its almost complete stop - stasis. Such changes are associated with exposure to the histamine vessels and sharp acidotic changes in the area of inflammation. Otherwise, the described changes are called term. "hyperemia". Local heat associated with increased catabolic reactions with energy release. Local temperature rise is usually determined by the back of the hand, comparing the sensations obtained with the sensations on palpation outside the painful focus. Swelling tissue caused by changes in the permeability of the vascular wall for plasma and uniform elements blood, as well as increased hydrostatic pressure in the capillaries. The increased permeability of the vascular wall mainly concerns capillaries and small veins. The liquid part of the plasma, which is sweating from the vessels, together with the migrating leukocytes and, quite often, the erythrocytes released by diapedesis form an inflammatory exudate. The bulk of it consists of neutrophilic leukocytes. Swelling is usually determined visually. In doubtful cases, measurements are made (limb circles, for example). Pain. The presence of pain and pain during palpation in the area of the focus is a characteristic sign of purulent diseases. It should be remembered that palpation should be done carefully enough so as not to cause negative feelings in the patient. Dysfunction. connected with both development pain syndrome, and with edema. It is most pronounced when the inflammatory process is localized on the limb, especially in the area of the joint. GENERAL SYMPTOMS The main clinical manifestations of the general reaction in purulent diseases are symptoms of intoxication, expressed in varying degrees. a) Clinical manifestations of intoxication -usually patients complain of feeling hot, chills, headache, general malaise, weakness, weakness, poor appetite, and sometimes delayed stool. They have an increase in body temperature (sometimes up to 40 ° C and above), tachycardia, shortness of breath. Patients are often covered with sweat, inhibited. Characteristic is the temperature change during the day by more than 1, 5-2 ° C - the temperature in the morning is normal or subfebrile, and in the evening it reaches high level (up to 39-40 ° C). Sometimes in patients the spleen and liver are enlarged, the icteric staining of the sclera appears. With a strongly pronounced general reaction of the organism to a surgical infection, all the listed changes appear in a sharp form. b) Changes in laboratory data. Changes in the clinical analysis of bloodall purulent surgical diseases are characterized by the presence of leukocytosis, leukocyte shift to the left, increased ESR. By shifting the formula to the left is understood neutrophilia (an increase in the percentage of neutrophils), as well as exceeding the normal level of band-leukocytes (more than 5-7%) and the appearance in the peripheral blood of immature (young) forms of leukocytes (adolescents, myelocytes). A relative decrease in the number of lymphocytes and monocytes is usually noted. The absolute decrease in lymphocytes and monocytes is an unfavorable sign and indicates the depletion of protective mechanisms. Increased ESR is usually observed within 1-2 days from the onset of the disease, and is restored 7-10 days after the relief of acute inflammatory events. Normalization of ESR usually indicates a complete elimination of the activity of the inflammatory process. With prolonged severe purulent processes, anemia is noted. Changes in the biochemical analysis of blood.Perhaps an increase in nitrogenous indicators (creatinine, urea), indicating the predominance of catabolic processes and insufficient kidney function. In complex and severe cases, the blood levels of the proteins of the acute phase (C-reactive protein, ceruloplasmin, haptoglobin, etc.) are determined. During long-term processes, there are changes in the protein fractions (a relative increase in the number of globulins, mainly due to g-globulins) It is also important to monitor blood glucose levels, as purulent diseases often develop on the background of diabetes. Sowing blood for sterilityUsually performed at a height of fever and helps diagnose sepsis (bacteremia). Changes in urine testsChanges in urine tests develop only with extremely severe intoxication and are called "Toxic bud". Note proteinuria, cylindruria, sometimes leukocyturia. Acute phase proteins - these are immunomodulators, proteins with direct or indirect bactericidal and (or) bacteriostatic action, inflammatory mediators, chemoattractants and nonspecific opsonins, primary alterations inhibitors, the synthesis of which grows in the liver during the acute period of inflammation after a certain spread of its focus within healthy tissues. These include proteins that migrate during electrophoresis in a gel in his region alpha-1 and alpha-2: alpha-1-antitrypsin, alpha-1 acid glycoprotein, amyloid A and P, antithrombin III, C-reactive protein, inhibitor C-1 esterase, NW complement fraction, cerulloplasmin, transferrin, haptoglobulin, orosomuoid, plasminogen. Acute phase response - these are changes in the tissues, organs and systems of the whole organism, developing as a result of the distant effect of inflammatory mediators, primarily of the Central Committee. In damaged tissue, pro and anti-inflammatory cytokines are activated. The proinflammatory group of the CK include IL1α, β, IL6, IL8, TNFα, β, IFα, β, granulocyte and monocytic colony-stimulating factors (g, MKSF) and some others. These mediators contribute to the development of the inflammatory process. Anti-inflammatory CC (IL4, IL5, IL10, IL13, IL18, transforming growth factors α, β (TGFα, β) counteract pro-inflammatory, limit damage and promote tissue repair, optimize the immune status of the body. Alteration Primary alteration - This is a set of changes in metabolism, physicochemical properties, structure and function of cells and tissues under the influence of the direct influence of etiological factor B. Primary alteration as a result of the interaction of etiological factor with the body is preserved and causes inflammation even after this interaction is terminated. The reaction of the primary alteration as if prolongs the action of the cause B. The causative factor itself may no longer be in contact with the body. Secondary alteration - occurs under the influence of a phlogogenic stimulus, as well as factors of primary alteration. If the primary alteration is the result of the direct action of the inflammatory agent, then the secondary does not depend on it and can continue even when this agent no longer has an effect (for example, upon radiation exposure). The etiological factor was the initiator, the trigger mechanism of the process, and then V. will proceed according to the laws peculiar to the tissue, organ, body as a whole. The action of the phlogogenic agent is manifested primarily on cell membranes, including lysosomes. When damaged by lysosomes, enzymes (acid hydrolases) are released that can break down various substances that make up the cell (proteins, nucleic acids, carbohydrates, lipids). Further, these enzymes, with or without an etiological factor, continue the process of alteration, as well as destruction, with the result that products of limited inflammatory mediators.Released under the influence of a damaging agent, mediators change a variety of processes occurring in tissues - vascular tone, permeability of their walls, emigration of leukocytes and other blood cells, their adhesion and phagocytic activity, cause pain, etc. Complex physical and chemical changes includes acidosis (due to impaired tissue oxidation and accumulation of oxidized products in tissues. First, it is compensated by buffer mechanisms, then it becomes decompensated. As a result, the exudate pH decreases. Along with increased acidity, pressure increases in the inflamed tissue), hyperionia (accumulation in source B ions K +, Cl -, NRA 4 from dying cells), disionium (changes in the ratio between individual ions, for example, an increase in the K + / Ca 2+ coefficient), hyperosmia, hyperoncution (due to icheniem protein concentration, its dispersion and hydrophilicity). The transport of fluid into the tissue depends on the physicochemical changes that occur on both sides of the vascular wall. In connection with the release of protein from the vascular bed, its amount outside the vessels increases, which contributes to an increase in oncotic pressure in the tissues. At the same time, in the hearth of V., under the influence of lysosomal hydrolases, the expansion of protein and other large molecules into smaller ones occurs. Hyperconia and hyperosmia in the focus of alteration create an influx of fluid in the inflamed tissue. This is facilitated by the increase in intravascular hydrostatic pressure due to changes in blood circulation in the outbreak B. 23. Dynamics of vascular reactions and changes in blood circulation during V.'s development of a stereotype: first there is a short-term reflex spasm of orteriole and precapillary blood flow with slowing down, then, replacing each other, arterial and venous hyperemia, prestasis and stasis develops to stop blood flow. Arterial hyperemia i is the result of the formation in the center of V. a large number of vasoactive substances - mediators V., which suppress the automaticity of the smooth muscle elements of the wall of arterioles and precapillaries, causing them to relax. This leads to an increase in arterial blood flow, accelerates its movement, opens previously not functioning capillaries, increases the pressure in them. In addition, the adductor vessels expand as a result of the “paralysis” of vasoconstrictors and the dominance of parasympathetic influences on the vessel wall, acidosis, hypercalium ionia, a decrease in the elasticity of the surrounding vessels. connective tissue. Venous hyperemia arises from a number of factors that can be divided into three groups: 1) blood factors, 2) vascular wall factors, 3) factors of surrounding tissues. The factors associated with blood include the regional arrangement of leukocytes, the swelling of red blood cells, the release of liquid blood into the inflamed tissue and the thickening of blood, the formation of microthrombus due to the activation of Hagemann factor and a decrease in heparin content. The influence of factors of the vascular wall on the venous hyperemia is manifested by swelling of the endothelium, as a result of which the lumen of small vessels narrows even more. Altered venules lose their elasticity and become more pliable to the compressive action of the infiltrate. And, finally, the manifestation of tissue factors consists in the fact that a hundred edematous tissue, squeezing the veins and lymphatic vessels, contributes to the development of venous hyperemia. With the development of the prestatic state, the pendulum-like movement of blood is observed - during systole it moves from the arteries to the veins, during the distal - in the opposite direction. Finally, the movement of blood can completely stop and develop. stasis, the consequence of which may be irreversible changes in blood cells and tissues. The output of the liquid part of the blood in the interstitium of the hearth V. - actually exudationoccurs as a result of a sharp increase in the permeability of the histohematogenous barrier and, as a consequence, an increase in the filtration process and microvesicular transport. The exit of liquid and the substances dissolved in it is carried out in places of contact of endothelial cells. The gaps between them may increase with the expansion of blood vessels, with the contraction of contractile structures and rounding of endothelial cells. In addition, endothelial cells are able to “swallow” the smallest droplets of liquid (micropynocytosis), transport them to the opposite side and throw them into the surrounding medium (extrusion). Leukocyte emigration (leukodiapedez) - the output of leukocytes from the lumen of blood vessels of the v / w vascular wall into the surrounding tissue. This process is accomplished in the norm, but with V. it acquires a much larger scale. The meaning of emigration is that a sufficient number of cells that play a role in the development of V. accumulate in V.'s focus (phagocytosis, etc.). Acute inflammation skin begins with the expansion of blood vessels, their overflow with red blood cells with a slightly increased admixture of leukocytes. Very soon, swelling of the vascular lining of the endothelium and the exit of the liquid and formed elements of the blood into the circulatory tissue joins. Due to the leakage of the liquid components of the blood, inflammatory edema develops in a larger or smaller space, characteristic signs which is a rarefaction of the fibrous stroma of the skin, swelling and weakening of the ability to dye connective tissue fibers. As for the cellular elements leaving the bloodstream in case of acute inflammation, here it is a question of leukocytes and first of all polymorphonuclear leukocytes. Among the polymorphonuclear leukocytes are distinguished: basophils; acidophilus (or eosinophils); neutrophils. The last among polymorphonuclear leukocytes are the most. During acute inflammation, the damaged capillary walls are often torn, and blood is poured into the surrounding tissue; more or less hemorrhage is obtained. In the area of the burnt tissue, we meet other cells, but they are comparatively smaller. These are lymphocytes, fibroblasts, polyblasts, occasionally Ehrlich mast cells and Unna's plasma cells. Fibroblasts especially increase in the number in the final stage of acute inflammation, during the period when the restoration of the skin damaged by the inflammation of the stroma begins. Polyblasts, also called macrophages (Swordsmen) or histiocytes, are active mesenchyme cells that absorb the pathological products of inflamed tissue: scraps of broken tissue, pieces of elastic fibers, fat drops, etc. The involvement of the skin stroma in the acute inflammatory process is far from always limited to the development in it of the above-described inflammatory edema. Very often, when exposed to a more or less energetic harmful agent, it comes to rebirth, dissolving and completely destroying in one or another area of all the tissues of the skin, including hair bags, sebaceous and sweat glands. In such cases, a cavity is obtained, sometimes performed by a huge number of neutrophils, an abscess.
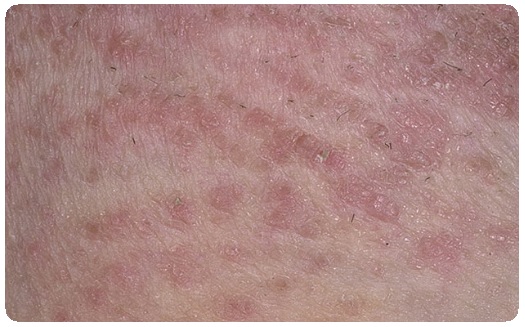
Chronic skin inflammationChronic inflammation of the skin also begins with the expansion of blood and lymphatic vessels, with swelling of the endothelium, swelling of the surrounding tissue and the release of blood cells into it. But soon this initial resemblance to the picture of acute inflammation gives way to a whole series of peculiar changes. The vascular endothelium often undergoes more or less significant proliferation, sometimes very pronounced. From the vessels mainly lymphocytes, not neutrophils. They accumulate in the inflammatory tissue, in significant amounts and, together with breeding fibroblasts, give rise to inflammatory infiltrate. The latter can reach a considerable thickness and by its pressure contribute to the destruction or atrophy of the skin stroma to one degree or another, which has also undergone inflammatory and edematous changes. The infiltrate in some cases is retained in the nearest circumference of the blood vessels, surrounding them in the form of a clutch, then we are talking about perivascular infiltration. In others, it accumulates in the form of more or less limited nests — nest infiltration, it can finally penetrate the skin over a considerable space continuously, completely, it is diffuse infiltration.
The composition of cellular elements of infiltration in chronic inflammation is much more diverse than in acute. It primarily contains lymphocytes, quite similar to blood lymphocytes, then polyblasts - large cells of polygonal shape, with a large number of reticular protoplasm, with a large round or oval core, well perceiving the main dyes. Often vacuoles containing various inclusions are visible in polyblasts: fat droplets, pigment grains, fragments of dead cells. Further, the morphologically original plasma cells (Plasmazellen) of Unna and the fat (Mastzellen) of Ehrlich are original. The former appear to be of various sizes and various shapes - a round, polygonal, oval cells with a mostly eccentrically located, large, spherical or oval nucleus with the original chromatin position in it: it is often located on the periphery of the nucleus in the form of more or less large grains. In the center of the nucleus lies the nucleolus, if we connect the mental lines of chromatin grain with the nucleolus, it sometimes turns out the wheel spokes. The basophilic protoplasm of these cells appears lumpy, according to Unna-Pappenheim, it is stained with pyronin in a raspberry-red color, and with polychrome methylene blue - in deep blue.
Fat cells of Ehrlich are very diverse in shape, often elongated, often equipped with more or less long processes. The protoplasm of their coarse grains, and the grains of its polychrome methylene blue are colored megachromatically in a purple-red color. Kernels mast cells either resemble plasma nuclei, they are very similar to elongated-oval nuclei of fibroblasts. Fibroblasts, a frequent component of the inflammatory infiltrate, have an elongated body, passing into long ribbon-like fiber processes, and very intensely stained spindle-shaped nuclei. More rarely, however, quite often, epithelioid cells are found in the infiltration, so named for their external similarity to the epithelium (in shape, properties of the nucleus, relative position, and relation to coloring matter). Unlike epithelium, they do not have protoplasmic fibers; their protoplasm is coarse-grained, crumbly. The nucleus has the appearance of a vesicle located predominantly in the center of the cell; it is stained somewhat more intensely than epithelial nuclei. The question of the origin of epithelioid cells is still open. Apparently, giant cells are very close genetically to epithelioid cells. In the infiltration of chronic inflammation, they have the form of ovoid large formations, sometimes elongated quadrangles with rounded corners, sometimes completely irregular. Their nuclei, very similar to the nuclei of epithelioid cells, are located mostly on the periphery, parietal. Protoplasm, fine-grained or homogeneous, is stained somewhat stronger than in epithelioid elements. Often there are vacuoles and various inclusions.
The quantitative interrelationships of the listed cellular elements of a chronic inflammatory infiltrate are far from the same, not all of them are also always present. Sometimes, however, the composition and location of the cellular infiltrate due to other symptoms (for example, the state of the blood vessels, the nature of its evolution) are represented to a certain extent typical of this or that suffering of the skin. For example, numerous giant cells in conjunction with epithelioid nests are often found in the tuberculous process. Infiltration consisting of large clusters of almost exclusively plasma cells is a frequent occurrence in papular syphilides (pure plasma). Changes in the epithelial region of the skinChanges in the epidermis are due to the defeat of epithelial cells with incomplete differentiation, i.e. the cells of the malpighian layer. Cells completely differentiated as cells of the stratum corneum are not capable of any further transformations in the order of a biological process, but they can undergo various transformations under the influence of chemical, physical and other agents of the same type as happens in reactions with dead tissue. Pathologically altered cells of the malpighian layer continue their development in an abnormal way, which is revealed by an anomaly in the structure of the epidermis. Changes in the epidermis as a whole and its individual elements are extremely diverse. The weak effect on the epidermis has a stimulating effect, causing its proliferation. Histologically, this is manifested by enhanced reproduction of cells of the basal layer, as evidenced by numerous mitosis. The result of proliferation is a thickening of the malpighian layer - uniform (diffuse) or in the form of cords, jutting into the skin itself (acanthosis). Thickening of the stratum corneum (hyperkeratosis) usually accompanies the excessive development of the granular layer. The incorrectness of keratinization may be reflected in the fact that the cells lose their ability to produce keratogialin. Flattening and not horny enough, they retain the nucleus (on a section of the rod-shaped form). This phenomenon is called parakeratosis.
The reaction of the epidermis to the harmful effects can also be detected by an increase in the volume of epithelial cells, weaker staining of them, lack of structure, the disappearance of the intercellular spaces, close contact of neighboring affected cells. This phenomenon is usually called cloudy swelling, or parenchymal edema. The formation in the cells of the malpighian layer of vacuoles in the form of a narrow rim near the nucleus or in the form of a large cavity, which occupied almost the entire cell and displaced the pyknotic semi-lunar form and the nucleus and protoplasmic remains to the cell membrane, known as vacuolar degeneration (alteration cavitaire). Intercellular edema or spongiosis, i.e. accumulation in the intercellular spaces of serous fluid in excess of the norm, can also be detected in the pathological state of the cells. The increased amount of fluid in the intercellular edema causes the expansion of the spaces between the cells and the elongation of the intercellular bridges, as a result of which the affected area becomes similar to a sponge, hence the name “spongiosis”. With a significant accumulation of fluid breaks intercellular bridges and the formation of bubbles. At the same time, individual cells or groups of them are separated from the rest of the epithelium and undergo degeneration. Bubbles in the epidermis are also formed as a result of the dissociation of epithelial cells as a result of a peculiar degeneration, accompanied by the disappearance of the intercellular bridges and the transformation of cells freely lying in the cavity of the bladder into homogeneous spherical formations (the so-called ballooning degeneration). With such a lesion sometimes there is a direct division of the nucleus and the formation of giant epithelial cells.
In addition to changes in the cellular elements of the malpighian layer and fluid flow (exo-serosis), infiltration of cells of the infiltrate (exocytosis), single or in the form of small clusters (miliary ulcers) occurs in the epidermis. The admixture of neutrophils to the contents of serous vesicles causes the transformation of serous vesicles into serous purulent or purulent (pustules). The formation of bubbles in the stratum corneum does not occur, but the bubbles that are in the malpighian layer gradually move outwards as the underlying epidermis develops and when the cornification of the latter occurs in the stratum corneum, where they undergo changes and are part of the flakes and crusts. Send your good work in the knowledge base is simple. Use the form below.Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you. abstractin general surgery« Inflammatory diseases»Is done by a studentMoscow 20091. Inflammation2. Phases of inflammation3. Classification of inflammations4. Clinical manifestations and features of the survey 5. General principles of treatment 6. The meaning and outcome of inflammationLiterature1. InflammationInflammation- complex local protective and adaptive response of the body to tissue damage by various pathogenic factors. This is a complex reaction developed in the course of phylogenesis and the evolution of the animal world, arising in response to an aggressive stimulus and characterized by a complex of alternative, exudative and proliferative processes. This, mainly local process, in one way or another involves the whole organism and, above all, such systems as the immune, endocrine and nervous systems. External signs of inflammation have been known for a long time. They are formulated in the famous pentad Celsus - Galen. These are swelling (tumor), redness (rubor), fever (calor), pain (dolor) and impaired function (functio laesa). Although these symptoms have been known for over 2000 years, they have not lost their significance today; over time, only their explanation changed. Purulent-inflammatory diseases are infectious in nature, they are caused by various types of pathogens; gram-positive and gram-negative, aerobic and anaerobic, spore-forming and non-spore-forming and other types of microorganisms, as well as pathogenic fungi. Under certain conditions favorable for the development of microorganisms, the inflammatory process may be caused by conditionally pathogenic microbes. The group of microbes that cause inflammation is called microbial association. Microorganisms can penetrate into the wound, into the zone of tissue damage from the external environment - exogenous infection or from the foci of microflora in the body itself - endogenous infection. 2. Phases of inflammation Morphologically, any inflammatory reaction composed of three closely related and consistently developing phases: alterations, exudations and proliferations. Alteration- tissue damage, manifested dystrophic, necrotic and atrophic changes; determines the initial phase of inflammation. The primary alteration is due to the direct effect of the damaging factor on the tissue with a change in its metabolism, structure and function. Secondary alteration occurs as a result of exposure to the decay products of cells and tissues after primary alteration, innervation disorders, blood circulation and immune reactions. In biochemical terms, primary and secondary alterations are characterized by metabolic disorders, predominance of catabolic processes, depolymerization and decomposition of protein-carbohydrate, protein-fat and protein-mineral complexes, accumulation of biologically active compounds and decomposition products with an increase in osmotic pressure and oncotic voltage, electrical potential and the development of acidosis. In this phase of inflammation, mediators (mediators) are excreted - biologically active chemicals that play the role of a triggering mechanism for inflammation and determine the whole subsequent picture of the inflammatory response as you further highlight. By origin, mediators are divided into two groups: tissue (cellular) and plasma. Sources of tissue, or cellular mediators are effector cells: labrocytes, basophilic and neutrophilic granulocytes, platelets ,. A major role is also played by the decay products of nucleic acids, hyaluronidase, lysosomal enzymes and other biologically active compounds of cells. Plasma neurotransmitters occur when three blood plasma systems are activated: kinima, blood coagulation and complementary. Exudation (from Lat. exsudatio - bleeding) occurs immediately after the alteration and release of mediators. Characterized by a complex of vascular changes, consistently developing in inflammation in the form of a series of stages: the reaction of the microvasculature with changes in the rheological properties of blood; increased vascular permeability of the microvasculature; proper exudation of the constituent parts of the blood plasma; emigration of blood cells; phagocytosis; the formation of exudate and inflammatory cellular infiltrate. Proliferation (from Lat. Proles - descendant, fero - wear, create) - the final phase of inflammation with the restoration of damaged tissue or scar formation. In this phase of inflammation as a result of alterative and exudative processes, under the influence of biologically active substances, anabolic processes are stimulated, RNA and DNA synthesis in cells, specific enzymatic and structural proteins, histiogenic and hematogenous cells proliferate. Proliferating fibroblasts synthesize the main substances of the connective tissue - tropocollagen (the precursor of collagen) and collagen, turn into mature cells - fibrocytes. Argyrophilic and collagen fibers are formed, granulation tissue with a large number of newly formed capillaries and young cells is transformed into fibrous connective tissue that replaces dead tissue or serves as a barrier between healthy and inflamed parts of the organ. During inflammation in the process of proliferation, complete or incomplete regeneration occurs, not only connective tissue, but also other damaged tissues, atrophied and necrotic parenchymal cells, epithelium are replaced, new vessels differentiate, nerve endings and nerve connections are restored, as well as cells providing local hormone and immune homeostasis. 3. Inflammation classification The classification is based on a number of principles. I. Depending on the etiological factor are distinguished: 1) not specific, or banal (polyetiological); 2) specific inflammation. Ii. According to the predominance of one of the components of the inflammatory reaction, regardless of the reason, there are: 1) alterative (parenchymal); 2) exudative; 3) proliferative (productive). Depending on the nature and other features, each type is divided into forms and types. Iii. Downstream there are: acute, subacute and chronic inflammation. Vi. Depending on the state of reactivity of the body and immunity, inflammations are distinguished: allergic, hyper-allergic (immediate or delayed type hypersensitivity reactions), hypoergic, immune. V. The prevalence of the inflammatory response: focal, diffuse, or diffuse. When taking into account the characteristics of the clinical course and the nature of changes in the focus of inflammation, acute and chronic forms are distinguished from all types of surgical infection. 1. Acute surgical infection: a) purulent; b) putrid; c) anaerobic; d) specific (tetanus, anthrax, etc.). 2. Chronic surgical infection: a) nonspecific (pyogenic); b) specific (tuberculosis, syphilis, actinomycosis, etc.). In each of these forms, there may be forms with a predominance of local manifestations (local surgical infection) or with a predominance of general phenomena with a septic course (general surgical infection). Purulent surgical infection is distinguished by etiological sign, localization, clinical manifestation of inflammation. 4. Clinical manifestations and features of the survey Clinical manifestations of purulent inflammatory diseases made up of local and common symptoms. Local manifestations of inflammation are determined by the stage of development, the nature and localization of the inflammatory process. Thus, the superficial foci of inflammation (purulent-inflammatory diseases of the skin, subcutaneous tissue of the mammary gland, muscles, etc.) or foci located deep in the tissues, but with involvement of the integuments in the inflammatory process, are characterized by classical signs of inflammation - redness due to inflammatory hyperemia, swelling, swelling, pain, increased local temperature and impaired organ function. The prevalence and severity of the inflammatory process determine the severity of local clinical manifestations. Inflammatory process in internal organs It has local signs characteristic of each disease, such as, for example, purulent pleurisy, peritonitis. During the clinical examination of patients with purulent-inflammatory diseases, the phase of the inflammatory process can be determined: palpable dense painful formation in the presence of other signs of inflammation indicates the infiltrative phase of the process in soft tissue and glandular organs, skin and subcutaneous tissue, breast, abdominal cavity. The softening of the infiltrate determined by palpation, a positive symptom of fluctuation, indicate a transition of the infiltrative phase of inflammation into a purulent one. Local clinical signs of progressive purulent inflammation are redness in the form of stripes on the skin (lymphangitis), dense cord-like painful condensations along the superficial veins (thrombophlebitis), and the appearance of dense painful condensations at the location of the regional lymph nodes (lymphadenitis). There is a correspondence between the severity of local symptoms of inflammation and the general clinical signs of intoxication: the progression of the inflammatory process is manifested by an increase in both local and general manifestations of inflammation and intoxication. Clinical signs of a general body response to inflammation are fever, chills, agitation or, on the contrary, patient lethargy, in extremely severe cases blackout, and sometimes loss of it, general malaise, weakness, increased heart rate, marked changes in the blood, signs of impairment liver function, kidney, lower blood pressure, stagnation in the pulmonary circulation. These symptoms may be pronounced or subtle, depending on the nature, prevalence, localization of inflammation and the characteristics of the reaction of the body. Body temperature during surgical infection can reach 40 ° C and higher, recurrent chills and headache occur, the percentage of hemoglobin and the number of red blood cells decrease sharply, the number of white blood cells increases. The amount of globulins increases in blood plasma and the amount of albumin decreases, appetite disappears in patients, bowel function is disturbed, stool retention appears, protein and cylinders are detected in urine. Developing intoxication leads to dysfunction of the blood-forming organs, resulting in anemization of the patient and significant changes in the composition of white blood: immature formed elements appear, there is a shift of leukocyte formula to the left (decrease in the number of segmented and increase in neutrophil stabs). For inflammatory processes characterized by a sharp increase in the rate of sedimentation of erythrocytes. It should be noted that, appearing at the beginning of the process, it is usually observed long after the elimination of inflammation. Sometimes the spleen, the liver are enlarged, and the icteric color of the sclera appears. With a strongly pronounced (hyperergic) general reaction of the body to a surgical infection, all the listed changes manifest themselves in a sharp degree; if the reaction is moderate or weak, they are moderate or even barely noticeable. However, any local inflammatory process is accompanied by general manifestations that, during a purulent infection, have a clinical picture that is very similar to sepsis and some infectious diseases (typhoid, brucellosis, paratyphoid, tuberculosis, etc.). Therefore, such patients need a thorough clinical examination, one of the important goals of which is to identify the primary suppurative focus, the entry gate for pyogenic microorganisms. In cases of severe generalized reactions in patients with a local inflammatory process, it is necessary not only to remember the possibility infectious disease, but also by repeated blood cultures to establish the presence or absence of bacteremia. Detection of bacteria in the blood, especially in the absence of clinical improvement after surgical treatment of the primary site of infection, indicates the presence of sepsis, and not just a general reaction to the local purulent process. The main difference of the general reaction of the organism to the purulent process from sepsis is that all its symptoms dramatically subside or disappear when the pus is opened and conditions for good drainage are created; in sepsis, symptoms almost do not change after that. Determining the degree of the general reaction to a local purulent infection is of great importance for the correct assessment of the patient’s condition, the nature of the development of inflammation and the prognosis of possible complications. The clinical signs of endogenous intoxication depend on the degree of its severity: the expression of intoxication, the harder it is manifested. With a mild degree of intoxication, paleness is noted skin coverin severe cases the skin is earthy; determined by acrocyanosis, facial flushing. Pulse frequent - up to 100-110 in 1 min, in severe cases, more than 130 in 1 min, decreases arterial pressure. Shortness of breath develops. An important indicator of intoxication is a violation of the functions of the central nervous system: from mild euphoria at first to lethargy or mental agitation during the development of toxemia. The definition of diuresis is important in assessing the severity of intoxication: in severe intoxication, the amount of urine decreases, in extremely severe cases, acute renal failure develops with severe oligouria or even anuria. From laboratory tests characterizing intoxication, an increase in the blood level of urea, necrotic bodies, polypeptides, circulating immune complexes, and proteolytic activity of blood serum is important. Severe intoxication is also manifested by increasing anemia, a shift to the left of the leukocyte formula, the appearance of the toxic granularity of the blood cells, the development of hypo - n dysproteinemia. To clarify the diagnosis of inflammatory diseases using special methods of research - puncture, x-ray, endoscopic methods, laboratory clinical and biochemical studies of blood, urine, exudate. Microbiological studies allow not only to determine the type of pathogen, its pathogenic properties, but also to identify the sensitivity of microorganisms to antibacterial drugs. The determination of the immunological status in order to conduct targeted, selective immunotherapy is important in a comprehensive examination of a patient with a purulent-inflammatory disease. Timely and complete surgical treatment of injuries and acute surgical diseases in combination with rational anthbiotic therapy not only contributed to reducing the number of patients with purulent infection, but also significantly changed the classical course of purulent diseases. Noted changes of the known clinical manifestations of the purulent process, especially with the hidden location of the lesion in the abdominal, thoracic cavities, etc., can make the diagnosis very difficult. Only a comprehensive examination of patients with purulent-inflammatory diseases allows you to establish the diagnosis of the disease, determine the nature and extent of the inflammatory process. 5. General principles of treatment Treatment of inflammatory diseases is carried out taking into account the general principles of treatment and features of the nature and localization of the pathological process (cellulitis, abscess, peritonitis, pleurisy, arthritis, osteomyelitis, etc.). Basic principles of treatment with surgical infection: 1) etiotropic and pathogenetic orientation of therapeutic measures; 2) the complexity of the treatment: the use of conservative (antibacterial, detoxification, immunotherapy, etc.) and surgical treatment methods; 3) carrying out therapeutic measures, taking into account the individual characteristics of the organism and the nature, localization and stage of development of the inflammatory process. Conservative treatment. In the initial period of inflammation, medical measures are aimed at combating microflora (antibacterial therapy) and the use of means to influence the inflammatory process in order to achieve the reverse development or limit it. During this period, use of conservative means - antibiotics, antiseptic, anti-inflammatory and decongestants (enzymotherapy), physiotherapy: thermal procedures (heating pads, compresses), ultraviolet radiation, ultra-high-frequency therapy (UHF-therapy), electrophoresis of drugs, laser therapy, etc. Mandatory condition treatment is the creation of rest for a sick organ: immobilization of the limb, restriction of active movements, bed rest. In the initial period of inflammatory infiltration of tissues, novocaine blockades are used - circular (sheath) blockages of the extremities, retromammary blockades, etc. For the purpose of detoxification, they use infusion therapy, blood transfusions, blood-substituting fluids, etc. If the inflammatory process has passed into the purulent phase with the formation of an abscess without significant inflammatory changes in the surrounding tissues, the removal of pus and washing of the abscess cavity can be provided by conservative means — abscess puncture, removal of pus and rinsing of the cavity with antiseptic solutions, the cavity of the abscess can be drained the same conservative method of treatment using therapeutic punctures and drainage is used for the accumulation of pus in the natural body cavities: with purulent pleurisy, suppurative arthritis, pericarditis. Surgery. The transition of the inflammatory process in the purulent phase, inefficiency conservative treatment serve as an indication for surgical treatment. Due to the risk of localized purulent inflammation passing into a general purulent infection (sepsis), the presence of purulent lesions determines the urgency of the surgery. Signs of severe or progressive inflammation and the ineffectiveness of conservative therapy are high fever, increasing intoxication, and locally in the area of inflammation, purulent or necrotic tissue breakdown, increasing swelling of tissues, pain, adherent lymphangitis, lymphadenitis, thrombophlebitis. Surgery patients with purulent-inflammatory diseases is the main method of treatment. Surgical access (surgical incision) should be shortest and wide enough to ensure removal of pus and necrotic tissues and be located in the lower part of the cavity to ensure good outflow of discharge. postoperative period. In some cases, an abscess is opened by the needle - the abscess is preliminarily punctured, and after receiving pus, the needle is not removed and the tissue is dissected along it. For a more complete removal of necrotic tissue after their excision, a laser beam or ultrasonic cavitation is used. The cavity of the abscess is thoroughly washed with antiseptic solutions. The operation is completed drainage of the wound. 6. The value and outcome of inflammation The value of inflammation for an organism is determined by the fact that this complex biological reaction, developed in the course of a long evolution, has a protective-adaptive character to the effects of pathogenic factors. Inflammation manifests itself as a local process, but simultaneously develops and general reactions: the body mobilizes the nervous and humoral connections that regulate the course of the inflammatory response; metabolic processes and blood composition change; functions of the nervous and hormonal systems; body temperature rises. The nature and degree of manifestation of the inflammatory reaction are determined both by the etiological factor and by the reactivity of the organism, its immunity, the state of the nervous, hormonal and other systems with which the inflammation is in inseparable unity. In the body with reduced reactivity and immunodeficiency, weakened or severely depleted, there is a slight inflammatory reaction. The type and nature of inflammation depends on the type and age of the animal. Exodus inflammation depends on the elimination of the etiological factor that caused it, resorption or removal of exudate, dead cell and tissue elements, the biological potential of regeneration of the remaining intact tissues, strength and stability of acquired immunity. Full resolution of the inflammatory process associated with the elimination of the pathogenic stimulus, resorption of dead tissue and exudate, is characterized by morphofunctional restoration (regeneration) of structural tissue and cellular elements and organ in the area of inflammation. With full resolution, full recovery occurs, with infectious and invasive diseases - immunity. Incomplete resolution with incomplete recovery is observed in cases of long-term preservation of the pathogenic irritant in the inflamed tissues, in the presence of a large amount of exudate with significant injuries and in highly specialized tissues with a special rhythm of functioning. At the same time, in the focus of inflammation, pathological states are noted: atrophy, necrosis, stenosis or expansion (cysts) of the ducts of the glands, adhesions, adhesions, connective tissue scars, calluses and other processes that deform the organ. Thus, the inflammatory process leads to serious changes in the body, to the dysfunction of various organs and systems, which requires special therapeutic measures to prevent and eliminate developed intoxication. Literature1. Alpern D., E., Inflammation (Questions of Pathology), M., 1999; 2. Mechnikov I. I., Lectures on the comparative pathology of inflammation, M., 1987. Similar documentsCauses of inflammation. The general concept of alteration. Local signs inflammation. Changes in the amount and quality of the plasma proteins. The transition of an acute inflammatory process to chronic. The value of inflammation for the body. abstract, added on 11.03.2013 Essence and patterns of manifestation of homeostasis. The levels of self-regulation of the body. The stress response of the body to damage. General and local adaptation syndrome. The processes of emergency and long-term adaptation. Stages of alteration, exudation and proliferation. abstract added on 10/02/2009 The body's response to the cause that brought it out of the state of dynamic equilibrium. Stage exudation and infiltration. Cells of inflammatory infiltrate. Metabolic changes during inflammation. Immunological reaction, the protective mechanisms of the body. abstract, added 01/23/2009 The concept and features of the course of proliferation as the final phase of the development of inflammation, providing reparative tissue regeneration at the site of the alteration source. Principles of regeneration and factors affecting this process. Classification and types of inflammation. presentation added on 07/14/2014 Classification and causes of inflammatory diseases of the genital organs in women, their symptoms and manifestations. Etiology and pathogenesis, clinical presentation, diagnostic methods and treatment of inflammatory diseases lower divisions genital tract, pelvic organs. abstract, added 15.06.2014 The structure of periodontal diseases, their types and forms of manifestation, various inflammatory processes as their most common type. Directions and features of the study the problem of the main cause of most dental diseases. abstract, added 06/22/2014 Inflammatory diseases genitourinary system: general characteristics and types. Symptoms, methods of treatment and prevention of phimosis, paraphimosis, orchitis, cystitis. Possible complications infectious and inflammatory diseases, indications for surgical treatment. presentation added on 09/22/2013 The inflammatory process in the female genitals. Changes in blood circulation in the inflammation. Classification of inflammatory diseases of the genitals. The main factors contributing to the occurrence of bacterial vaginosis. Acute chronic adnexitis. presentation added on 11/17/2014 Factors affecting the development of acute suppurative inflammation of apocrine sweat glands. Symptoms and the process of flow of hydradenitis. Localization of inflammatory processes in the skin and subcutaneous retina. Essence of conservative and surgical treatment diseases. presentation added on 11/29/2015 The study of coagulation factors. Theory of the three-phase process of hemocoagulation. Pathogenetic classification of hemorrhagic diseases. Forms of hemophilia, clinical manifestations, the frequency of the disease. Methods of treatment and prevention. |
| Read: |
|---|
New
- Which leaves blush first in autumn
- Sequence of procedures
- The program of intensive moisturizing of the skin on cosmetics bark
- What you need for acrylic powder
- What does owl mascot mean
- Analyzes for pancreatitis: what research should be done and what indicators show
- Owl - a talisman to attract money and good luck
- What bird screams at night with a kitten's voice?
- Cholesterol and stress
- Manicure at home