Site sections
Editor's Choice:
- Technology and step-by-step instructions for nail gel: steps, rules, process
- White spots on the nails, reasons for what to do, white spots on the nails and folk signs
- Available methods for rapidly increasing blood leukocytes
- Nail and skin fungus will not resist the coffee grounds
- Crocus furniture exhibition. Furniture exhibitions
- Owl tattoo on arm value
- The biggest members in the world
- Fractures of the phalanges of the foot photo
- What is “bad” and “good” cholesterol
- What to do if the skin around the nails dries
Advertising
| The internal environment of the body. Features of digestion in the colon. General properties of blood. Blood cells |
|
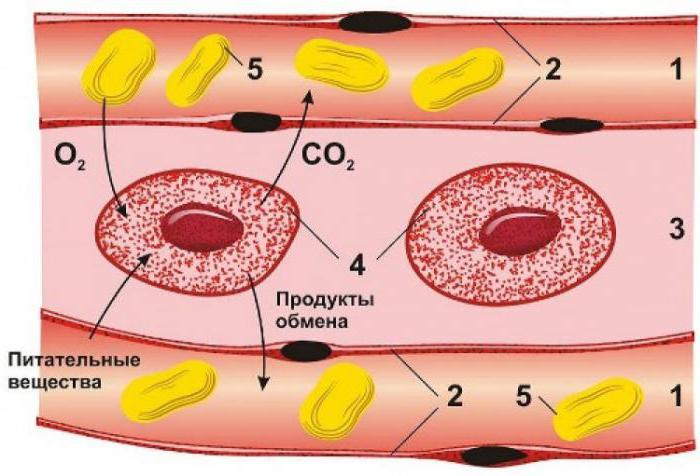
§28. Tissue fluid. Lymph In addition to blood, body fluid and lymph make up the internal environment of the body. Tissue fluid - a colorless, transparent liquid, which is formed from blood plasma and fills the intercellular space in the body. It penetrates here through the walls of blood vessels. In an adult it is about 1-1-20 liters. Between the tissue fluid and blood is constantly metabolism. The connection between cells and capillaries is carried out through the tissue fluid. Oxygen (O and a) and nutrients can enter the cell only in the form of solutions. Therefore, from the capillaries they first enter the tissue fluid and then into the cells of the organs. The concentration of carbon dioxide (CO,) formed in the cells, as well as the amount of water and other metabolic products are different in the cytoplasm of cells and tissue fluid. Therefore, metabolic products are first released from the cells into the tissue fluid, and from the tissue fluid they enter the capillaries. The substances necessary for the cells are delivered by the tissue fluid from the capillaries. Carbon dioxide and metabolic products of the cell emit into the tissue fluid, and then they enter the blood. Tissue fluid provides the relative constancy of the chemical composition of the cells of organs and tissues when the composition of the blood changes. Absorbing into lymphatic capillaries, the tissue fluid turns into lymph. Functions of tissue fluid, see table. 3 Lymph (from lat.lymph moisture) transparent yellowish liquid (liquid connective tissue), flowing through human lymphatic vessels and nodes. Lymph is an integral part of Table 3. Internal heated the body of an adult her body environment. It is formed from the tissue fluid. The composition of mineral salts, it is similar to blood plasma. The chemical composition of lymph: 95% - water; 3 4% - proteins; 0.1% glucose; 0.9% mineral salts. About 1.5 liters of lymph is produced per day in humans. Compared with plasma in the lymph less protein, and therefore its viscosity is less. Lymph has the ability to coagulate. Like blood, it is in constant motion. Leukocytes in the lymph are presented lymphocytes. They are actively involved in the immune reactions of the body, make up 19-30% of all leukocytes. Lymphocytes are small cells, very sensitive to the penetration of microbes. Lymph functions: returns tissue fluid to the circulatory system; filters out harmful microbes and foreign particles that enter the body; promotes fat absorption. In addition to the main ones - blood, tissue fluid and lymph (Table 3), the articular, pericardial, cerebrospinal and pleural (pulmonary) fluids are also referred to as body fluid. Tissue fluid, lymph, lymphocytes. BUT 1. What is tissue fluid? Where is it kept? 2. What are the functions of tissue fluid? 3. What does lymph come from? What substances are included in its composition? AT 1. What is tissue fluid formed from? How does it penetrate the intercellular space? 2. What are the cells called lymphocytes? 3. What are the functions of lymphocytes? WITH 1. What is lymph? Describe its composition. 2. What are the functions of lymph. 3. What refers to the internal environment of the body? Characterize briefly the features of each of its components. 1. Blood is the internal environment of the body. Blood functions The composition of human blood. Hematocrit. The amount of blood circulating and deposited blood. Hematocrit and blood counts in a newborn. General properties blood. Formed elements of blood. Blood and lymph are the internal environment of the body. Blood and lymph directly surrounds all cells, tissues and provides vital activity. The entire amount of metabolism occurs between cells and blood. Blood is a variety connective tissue, which includes blood plasma (55%) and blood cells or shaped elements (45%). Uniform elements are represented by erythrocytes (red blood cells 4.5-5 * 10 per 12 l), leukocytes 4-9 * 10 per 9 l, platelets 180-320 * 10 per 9 l. The peculiarity is that the elements themselves are formed outside - in the blood-forming organs, and why go into the blood and live for some time. The destruction of blood cells also occurs outside this tissue. Scientist Lang introduced the concept of the blood system, in which he included the blood itself, blood-forming and blood-destroying organs and the apparatus of their regulation. Features - the extracellular substance in this tissue is fluid. The bulk of the blood is in constant motion, due to what are humoral communication in the body. The amount of blood - 6-8% of body weight, this corresponds to 4-6 liters. A newborn has more blood. The mass of blood is 14% of body weight and by the end of the first year is reduced to 11%. Half of the blood is in circulation, the main part is placed in the depot and represents the deposited blood (spleen, liver, subcutaneous vascular systems, vascular systems of the lungs). For the body is very important to preserve blood. The loss of 1/3 can lead to the death of a ½ blood - a state incompatible with life. If the blood is subjected to centrifugation, the blood is divided into plasma and shaped elements. And the ratio of red blood cells to the total blood volume is called hematocrit (for men, 0.4-0.5 l / l, for women - 0.37-0.47 l / l ) .Sometimes expressed as a percentage. Blood functions -
Blood plasma Organic Inorganic Inorganic substances in plasma - Sodium 135-155 mmol / l, chlorine 98-108 mmol / l, calcium 2.25-2.75 mmol / l, potassium 3.6-5 mmol / l, iron 14-32 μmol / l 2. Physical and chemical properties of blood, their characteristics in children. Physico-chemical properties of blood
Osmotic pressure of blood is created by minerals and proteins. Moreover, 60% of osmotic pressure accounted for sodium chloride. Plasma proteins create an osmotic pressure of 25-40 mm. mercury column (0.02 atm). But despite its small size, it is very important for retaining water inside the vessels. A decrease in protein content in the blood will be accompanied by edema, since water starts to go out into the cage. Observed during the Great Patriotic War during the famine. The magnitude of the osmotic pressure is determined by the method of cryoscopy. Determine the temperature of the osmotic pressure. Lowering the freezing temperature below 0 - blood depression and blood freezing temperature - 0.56 C. - osmotic pressure with 7.6 atm. Osmotic pressure is maintained at a constant level. To maintain osmotic pressure, proper function of the kidneys, sweat glands and intestines is very important. Osmotic pressure of solutions that have the same osmotic pressure. As the blood is called isotonic solutions. The most common solution is 0.9% sodium chloride, 5.5% glucose solution .. Solutions with less pressure are hypotonic, large ones are hypertonic. Active blood reaction. Blood buffer system
3. Blood plasma. Osmotic pressure of blood. Blood plasma - a liquid yellowish opalescent liquid, which consists of 91-92% of water, and 8-9% - the residue is dense. It contains organic and inorganic substances. Organic - proteins (7-8% or 60-82 g / l), residual nitrogen - as a result of protein metabolism (urea, uric acid, creatinine, creatine, ammonia) - 15-20 mmol / l. This indicator characterizes the work of the kidneys. The growth of this indicator indicates renal failure. Glucose - 3.33-6.1 mmol / l - diabetes is diagnosed. Inorganic - salts (cations and anions) - 0.9% Plasma is a yellowish slightly opalescent liquid, and is a very complex biological medium, which includes proteins, various salts, carbohydrates, lipids, metabolic intermediates, hormones, vitamins and dissolved gases. It includes both organic and inorganic substances (up to 9%) and water (91-92%). Blood plasma is in close connection with body tissue fluids. A large number of metabolic products enter the blood from the tissues, but due to the complex activity of various physiological systems of the body, no significant changes occur in the plasma composition. The amount of proteins, glucose, all cations and bicarbonate is kept at a constant level and the smallest fluctuations in their composition lead to severe disruptions in the normal activity of the body. At the same time, the content of substances such as lipids, phosphorus, urea, can vary significantly, without causing noticeable disorders in the body. The concentration of salts and hydrogen ions in the blood is very precisely regulated. The composition of blood plasma has some fluctuations depending on age, sex, nutrition, geographical features of the place of residence, time and season of the year. Functional system of regulation of osmotic pressure. The osmotic pressure of the blood of mammals and humans is normally kept at a relatively constant level (Hamburger’s experience with the introduction of 7 l of 5% sodium sulfate solution into a horse’s blood). All this is due to the activity of the functional system of regulation of osmotic pressure, which is closely linked to the functional system of regulation of water-salt homeostasis, as it uses the same executive organs. In the walls of blood vessels there are nerve endings that respond to changes in osmotic pressure ( osmoreceptors). Their irritation causes excitation of the central regulatory structures in the medulla oblongata and the diencephalon. From there come teams that include certain organs, for example, the kidneys, which remove excess water or salts. From other executive agencies digestive tractin which there is both the excretion of excess salts and water, and the absorption necessary for the recovery of OD products; the skin, the connective tissue of which absorbs an excess of water when osmotic pressure decreases or gives it back to the latter when osmotic pressure increases. In the intestine, solutions of mineral substances are absorbed only in such concentrations that contribute to the establishment of normal osmotic pressure and the ionic composition of the blood. Therefore, when taking hypertonic solutions (British salt, sea water), the body is dehydrated due to the removal of water into the intestinal lumen. The laxative effect of salts is based on this. A factor capable of altering the osmotic pressure of tissues, as well as blood, is metabolism, because the cells of the body consume coarse-molecular nutrients, and instead release a significantly larger number of molecules of low-molecular metabolic products. From this it is clear why venous blood flowing from the liver, kidneys, muscles has a greater osmotic pressure than arterial pressure. It is not by chance that these organs contain the largest number of osmoreceptors. Especially significant changes in osmotic pressure in the whole body are caused by muscular work. With very intensive work, the activity of the excretory organs may be insufficient to maintain the osmotic pressure of the blood at a constant level and, as a result, it may increase. The shift of the osmotic pressure of blood to 1,155% NaCl makes it impossible to continue the work (one of the components of fatigue). 4. Plasma proteins. Functions of the main protein fractions. The role of oncotic pressure in the distribution of water between the plasma and the extracellular fluid. Features of the protein composition of plasma in young children. Blood plasma proteins represented by several fractions that can be detected by electrophoresis. Albumins - 35-47 g / l (53-65%), globulins 22.5-32.5 g / l (30-54%), are divided into alpha1, alpha 2 (alpha are transport proteins), beta and gamma ( protective bodies) globulins, fibrinogen 2.5 g / l (3%). Fibrinogen is a substrate for blood clotting. It forms a blood clot. Gamma globulins produce plasma cells of lymphoid tissue, the rest in the liver. Plasma proteins are involved in the creation of oncotic or coloid-osmotic pressure and are involved in the regulation of water metabolism. Protective function, transport function (transport of hormones, vitamins, fats). Participate in blood coagulation. Blood coagulation factors are formed by protein components. Possess buffer properties. In diseases there is a decrease in the level of protein in the blood plasma. The most complete separation of plasma proteins by electrophoresis. On electrophoregram, 6 plasma protein fractions can be distinguished: Albumins . They are contained in the blood of 4.5-6.7%, i.e. 60-65% of all plasma proteins accounted for albumin. They perform mainly nutritional-plastic function. No less important is the transport role of albumin, since they can bind and transport not only metabolites, but medications. With a large accumulation of fat in the blood, part of it is also bound by albumin. Since albumin has a very high osmotic activity, they account for up to 80% of the total colloid-osmotic (oncotic) blood pressure. Therefore, reducing the amount of albumin leads to disruption of water metabolism between tissues and blood and the appearance of edema. Albumin synthesis occurs in the liver. Their molecular weight is 70-100 thousand, so part of them can resemble the renal barrier and back sucked into the blood. Globulins usually accompanied by albumin and are the most common of all known proteins. The total amount of globulins in the plasma is 2.0-3.5%, i.e. 35-40% of all plasma proteins. By fractions, their content is as follows: alpha1 globulins - 0,22-0,55 g% (4-5%) alpha2 globulins - 0.41-0.71g% (7-8%) beta globulins - 0.51-0.90 g% (9-10%) gamma globulins - 0.81-1.75 g% (14-15%) The molecular weight of globulins is 150-190 thousand. The place of formation may be different. Most of them are synthesized in the lymphoid and plasma cells of the reticuloendothelial system. Part - in the liver. The physiological role of globulins is diverse. So, gamma globulins are carriers of immune bodies. Alpha and beta globulins also have antigenic properties, but their specific function is to participate in coagulation processes (these are plasma coagulation factors). This includes most of the blood enzymes, as well as transferrin, ceruloplasmin, haptoglobins and other proteins. Fibrinogen. This protein is 0.2-0.4 g%, about 4% of all plasma proteins. It is directly related to coagulation, during which it precipitates after polymerization. Plasma devoid of fibrinogen (fibrin) is called blood serum. With various diseases, especially leading to impaired protein metabolism, there are sharp changes in the content and fractional composition of plasma proteins. Therefore, the analysis of plasma proteins has diagnostic and prognostic value and helps the doctor to judge the extent of damage to organs. 5. Blood buffer systems, their significance. Blood buffer system(pH fluctuation 0.2-0.4 - very serious stress)
Any buffer system includes a weak acid and a salt formed by a strong base. NaHCO3 + HCl = NaCl + H2CO3 (H2O and CO2-is removed through the lungs) 6. Erythrocytes, their number, physiological role. Age fluctuations in the number of red blood cells. rhythm cells - the most numerous blood units, the content of which differs in men (4.5-6.5 * 10 per 12 l) and women (3.8-5.8). Non-nuclear highly specialized cells. They have the shape of a biconcave disc with a diameter of 7-8 microns and a thickness of 2.4 microns. This form increases its surface area, increases the stability of the membrane of red blood cells, with the passage of capillaries, it can be folded. Erythrocytes contain 60-65% of water and 35-40% is dry residue. 95% of the dry residue - hemoglobin - respiratory pigment. The remaining proteins and lipids account for 5%. Of the total mass of the erythrocyte, hemoglobin mass is 34%. The size (volume) of the erythrocyte is 76-96 femto / l (-15 degree), the average volume of the erythrocyte can be calculated by dividing the hematocrit by the number of erythrocytes per liter. The average hemoglobin content is determined by picograms - 27-32 pico / g - 10 v - 12. Outside, the erythrocyte is surrounded by a plasma membrane (a double lipid layer with integral proteins that permeate this layer and these proteins are glycophorin A, protein 3, ankyrin. On the inside membranes - spectrin proteins and actin. These proteins strengthen the membrane). Outside, the membrane has carbohydrates - polysaccharides (glycolipids and glycoproteins and polysaccharides carry the antigens A, B and W). Transport function of integral proteins. There are sodium-potassium atphase, calcium-magnesium atphase. Inside, red blood cells are 20 times more potassium, and sodium is 20 times less than in plasma. The packing density of hemoglobin is large. If erythrocytes in the blood have a different size, then this is called anisocytosis, if the form is different - okelocytosis. Red blood cells are formed in the red inert brain and then enter the blood, where they live for an average of 120 days. Erythrocyte metabolism is aimed at maintaining the erythrocyte form and at maintaining the affinity of hemoglobin for oxygen. 95% of the glucose absorbed by the erythrocytes is subjected to anaerobic glycolysis. 5% use the pentose phosphate pathway. A by-product of glycolysis is a substance 2,3-diphosphoglycerate (2,3-DFG) Under conditions of oxygen deficiency, this product is more formed. With the accumulation of DFG, the oxyhemoglobin oxygen release is lighter. Erythrocyte functions
The increase in red blood cells (physiological erythrocytosis) in the blood will contribute to physical exercise, food intake, neuro-psychological factors. The number of erythrocytes increases in mountain dwellers (7-8 * 10 per 12). With blood diseases - erythrimysia. Anemia - a decrease in the content of red blood cells (due to lack of iron, lack of absorption of folic acid (vitamin B12)). Counting the number of red blood cells. Produced in a special counting chamber. Camera depth 0.1 mm. Under the cover stele and the camera - a gap of 0.1 mm. On the middle part there is a grid - 225 squares. 16 small squares (side of a small square 1 / 10mm, 1/400 square, volume - 1/4000 mm3) Dilute blood 200 times with 3% sodium chloride solution. Red blood cells shrink. Such diluted blood is supplied under a cover glass in a counting chamber. Under the microscope, we count the number in 5 large squares (90 small), divided into small ones. The number of red blood cells = A (the number of red blood cells in five large squares) * 4000 * 200/80 7. Hemolysis of erythrocytes, its types. Osmotic resistance of erythrocytes in adults and children. The destruction of the erythrocyte membrane with the release of hemoglobin in the blood. The blood becomes transparent. Depending on the causes of hemolysis, it is divided into osmotic hemolysis in hypotonic solutions. Hemolysis can be mechanical. When shaking the ampoules, they may break, thermal, chemical (alkali, gasoline, chloroform), biological (blood group incompatibility). The stability of erythrocytes to the hypotonic solution varies with different diseases. The maximum osmotic resistance is 0.48-044% NaCl. The minimum osmotic resistance is 0.28 - 0.34% NaCl Erythrocyte sedimentation rate. Erythrocytes are retained in the blood in suspension due to small differences in the density of erythrocytes (1.03) and plasma (1.1). The presence of zeta potential on the erythrocyte. Red blood cells are in the plasma, as in a colloidal solution. A zeta potential is formed at the boundary between the compact and diffuse layer. This ensures that the red blood cells repel each other. Violation of this potential (due to the introduction of protein molecules into this layer) leads to the erythrocyte adhesion (coin columns). The particle radius increases, the segmentation rate increases. Continuous blood flow. The erythrocyte sedimentation rate of the 1st erythrocyte is 0.2 mm per hour, and in fact for men (3-8 mm per hour), for women (4-12 mm), for newborns (0.5 - 2 mm per hour). The erythrocyte sedimentation rate is subject to the Stokes law. Stokes studied the sedimentation rate of particles. Particle sedimentation rate (V = 2 / 9R in 2 * (g * (density 1 - density 2) / eta (viscosity in poise))) Observed at inflammatory diseaseswhen a lot of coarse proteins are formed - gamma globulins. They reduce zeta potential more and contribute to settling. 8. Erythrocyte sedimentation rate (ESR), mechanism, clinical significance. Age changes ESR. Blood is a stable suspension of small cells in a liquid (plasma). The property of the blood as a stable suspension is disturbed when the blood transitions to a static state, which is accompanied by cell sedimentation and is most clearly manifested by red blood cells. The noted phenomenon is used to evaluate blood suspension stability when determining the erythrocyte sedimentation rate (ESR). If you protect the blood from clotting, the shaped elements can be separated from the plasma by simple sedimentation. This has practical clinical significance, since the ESR varies noticeably in some conditions and diseases. Thus, ESR is greatly accelerated in women during pregnancy, in patients with tuberculosis, and in inflammatory diseases. When blood stands, erythrocytes stick together (agglutinate) with each other, forming so-called coin columns, and then conglomerates of coin columns (aggregation), which precipitate the faster, the greater their size. The aggregation of erythrocytes, their gluing depends on changes in the physical properties of the surface of erythrocytes (possibly with a change in the sign of the total charge of the cell from negative to positive), as well as on the nature of the interaction of erythrocytes with plasma proteins. The suspension properties of blood depend mainly on the protein composition of the plasma: an increase in the content of coarse proteins during inflammation is accompanied by a decrease in suspension stability and an accelerated ESR. The magnitude of the ESR depends on the quantitative ratio of plasma and red blood cells. In newborns, the ESR is 1-2 mm / hour, in men, 4-8 mm / hour, and in women, 6-10 mm / hour. ESR is determined by the Panchenkov method (see workshop). Accelerated ESR due to changes in plasma proteins, especially during inflammation, also corresponds to increased aggregation of erythrocytes in the capillaries. The predominant aggregation of erythrocytes in the capillaries is associated with physiological slowing down of the blood flow in them. It has been proven that in conditions of slow blood flow, an increase in the content of coarse proteins in the blood leads to a more pronounced aggregation of cells. Erythrocyte aggregation, reflecting the dynamism of the suspension properties of blood, is one of the oldest protective mechanisms. In invertebrates, erythrocyte aggregation plays a leading role in the processes of hemostasis; at inflammatory response this leads to the development of stasis (stop blood flow in the border areas), contributing to the delimitation of the center of inflammation. Recently, it has been proved that in ESR, it is not so much the charge of erythrocytes that matters, but the nature of its interaction with hydrophobic complexes of a protein molecule. The theory of neutralization of the charge of erythrocytes by proteins has not been proven. 9. Hemoglobin, its types in the fetus and newborn. Hemoglobin compounds with various gases. Spectral analysis of hemoglobin compounds. Oxygen transfer. Hemoglobin attaches oxygen at high partial pressure (in the lungs). There are 4 heme in the hemoglobin molecule, each of which can add an oxygen molecule. Oxygenation is the addition of oxygen to hemoglobin, since there is no process of changing the valence of iron. In tissues where low partial pressure hemoglobin gives oxygen - deoxykination. The combination of hemoglobin and oxygen is called oxyhemoglobin. The process of oxygenation goes stepwise. During oxygenation, the oxygen addition process increases. Cooperative effect - at the end of the oxygen molecules join 500 times faster. 1 g of hemoglobin adds 1.34 ml of O2. 100% blood saturation with hemoglobin - maximum percentage (volume) saturation 20ml per 100ml of blood. In fact, hemoglobin is saturated by 96-98%. The addition of oxygen also depends on the pH, on the amount of CO2, 2,3-diphosphonic glycerate (a product of incomplete oxidation of glucose). With the accumulation of its hemoglobin begins to give out oxygen more easily. Methemoglobin, in which iron becomes 3-valent (under the action of strong oxidizing agents, potassium ferricyanide, nitrates, bertolet salt, fenacitin) It cannot give oxygen. Methemoglobin is capable of binding hydrocyanic acid and other bonds, therefore, when poisoning with these substances, methemoglobin is injected into the body. Carboxyhemoglobin (Hb compound with CO) carbon monoxide is attached to hemoglobin to iron, but the affinity of hemoglobin to carbon monoxide gas is 300 times higher than to oxygen. If the air is more than 0.1% carbon monoxide, then hemoglobin is associated with carbon monoxide. 60% is associated with carbon monoxide (death). Carbon monoxide is found in exhaust gases, in furnaces, formed during smoking. Assistance to victims - carbon monoxide poisoning begins unnoticed. The person himself cannot move, his removal from this room is necessary and the provision of breathing is preferably a gas balloon with 95% oxygen and 5% carbon dioxide. Hemoglobin can join carbon dioxide - carbhemoglobin. The connection occurs with the protein part. The acceptor is the amine parts (NH2) - R-NH2 + CO2 = RNHCOOH. This compound is capable of removing carbon dioxide. The combination of hemoglobin with different gases has different absorption spectra. Restored hemoglobin has one wide band of the yellow-green part of the spectrum. In oxyhemoglobin, 2 bands are formed in the yellow-green part of the spectrum. Methemoglobin has 4 bands - 2 in yellow-green, in red and in blue. Carboxyhemoglobin has 2 bands in the yellow-green part of the spectrum, but this compound can be distinguished from oxyhemoglobin by adding a reducing agent. Since the carboxyhemoglobin compound is strong, the addition of a reducing agent does not add bands. Hemoglobin has an important function in maintaining a normal pH level. With the release of oxygen in the tissues hemoglobin attaches a proton. In the lungs, the proton of hydrogen is given to form carbonic acid. When hemoglobin is exposed to strong acids or alkalis, compounds with a crystalline form are formed and these compounds are the basis for confirming blood. Hemines, hemochromogens. Glycine and succinic acid are involved in the synthesis of parfirin (pyrrole ring). Globin is formed from amino acids by protein synthesis. In red blood cells that complete their life cycle hemoglobin breakdown also occurs. In this case, the gems are separated from the protein part. Iron is relaxed from the hemma, and bile pigments are formed from the hemma residues (for example, bilirubin, which will then be taken up by the liver cells). Hemoglobin is linked to glucuronic acid inside hepatocytes. Bilirubin Hyukuronit is excreted in the bile capillaries. With bile enters the intestine, where it undergoes oxidation, where it passes into urabillin, which is absorbed into the blood. Part of it remains in the intestines and is excreted with feces (their color is stercobillyn). Urrabillin gives color to the urine and is again taken up by the liver cells. Hemoglobin content in erythrocytes is judged by the so-called color indicator, or farb-index (Fi, from farb - color, index - indicator) - the relative value characterizing the saturation on average of one erythrocyte with hemoglobin. Fi - the percentage of hemoglobin and red blood cells, while for 100% (or units) of hemoglobin conditionally accept a value equal to 166.7 g / l, and for 100% of red blood cells - 5 * 10 / l. If a person has a hemoglobin and erythrocyte content of 100%, then the color index is 1. Normally, Fi varies between 0.75-1.0 and very rarely can reach 1.1. In this case, the red blood cells are called normochromic. If Fi is less than 0.7, then such red blood cells are undersaturated with hemoglobin and are called hypochromic. When Fi is more than 1.1, red blood cells are hyperchromic. In this case, the volume of the erythrocyte increases significantly, which allows it to contain a greater concentration of hemoglobin. As a result, a false impression is created, as if erythrocytes are supersaturated with hemoglobin. Hypo- and hyperchromia are found only with anemia. The determination of the color index is important for clinical practice, as it allows a differential diagnosis for anemias of various etiologies. 10. Leukocytes, their number and physiological role. White blood cells. These are nuclear cells without a polysaccharide membrane. Sizes - 9-16 microns The normal amount - 4-9 * 10 in 9l Education occurs in the red inert brain, lymph nodes, spleen. Leukocytosis - an increase in the number of leukocytes Leukopenia - reducing the number of leukocytes The number of leukocytes = B * 4000 * 20/400. Considered on the grid Goryaeva. The blood is diluted with 5% solution of acetic acid tinted with methylene blue, diluted 20 times. In an acidic environment, hemolysis occurs. Next, the diluted blood is placed in the counting chamber. Count the number in 25 large squares. Counting can be done in unseparated and divided squares. The total number of counted leukocytes will be 400 small. We learn how many leukocytes on average per one small square. Translated into cubic millimeters (multiplied by 4000). We take into account the dilution of blood 20 times. In newborns, the number on the first day is increased (10-12 * 10 per 9 l). By 5-6 years, comes to the level of an adult. The increase in leukocytes causes physical exercise, food intake, pain sensationsstressful situations. The number increases during pregnancy, with cooling. This is a physiological leukocytosis associated with the release of a larger number of leukocytes into the circulation. These are redistributive reactions. Daily fluctuations - less leukocytes in the morning, more in the evening. In infectious inflammatory diseases, the number of leukocytes increases due to their participation in protective reactions. The number of leukocytes may increase with leukemia (leukemia) General properties of leukocytes
11. Leukocyte formula, its clinical significance. B-and T-lymphocytes, their role. Leukocyte formula
A. Neutrophils 47–72% (segmented (45–65%), band (1–4%), young (0–1%)) B. Eosinophils (1-5%) B. Basophils (0-1%)
A. Lymphocytes (20-40%) B. Monocytes (3-11%) The percentage of different forms of leukocyte is leukocyte formula. Counting in a blood smear. Coloring according to Romanovsky. Out of 100 leukocytes, how many will fall on these varieties. In the leukocyte formula, there is a shift to the left (increase in young forms of leukocyte) and to the right (disappearance of young forms and the predominance of segmented forms) Shift to the right characterizes the inhibition of the function of the red inert brain, when new cells are not formed, but only mature forms are present. More unfavorable. Features features individual forms. All granulocytes have a high lability of the cell membrane, adhesive properties, chemotaxis, phagocytosis, free movement. Neutrophil granulocytes are formed in the red inert brain and live in the blood of 5-10 hours. Neutrophils contain lysosamic, peroxidase, hydrolytic, Sup-oxidase. These cells are our non-specific defenders against bacteria, viruses, and foreign particles. Their number at age of infection. The site of infection is approached through chemotaxis. They are capable of capturing bacteria by phagocytosis. Phagocytosis discovered Mechnikov. Absonins, phagocytosis-enhancing substances. Immune complexes, C-reactive protein, aggregated proteins, fibronectins. These substances cover foreign agents and make them "tasty" for leukocytes. In contact with an alien object - protrusion. Then there is a separation of this bubble. Then inside, it fuses with lysosomes. Further, under the influence of enzymes (peroxidase, adoxidase) neutralization occurs. Enzymes break down the foreign agent, but the neutrophils themselves die. Eosinophils. They phagocytize histamine and destroy it by the histaminase enzyme. Contain protein that destroys heparin. These cells are necessary to neutralize toxins, seize immune complexes. Eosinophils destroy histamine in allergic reactions. Basophils - contain heparin (anticoagulant action) and histamine (dilates blood vessels). Mast cellswhich contain on their surface receptors for immunoglobulins E. Active substances derived from arachidonic acid are platelet activating factors, thromboxanes, leukotrienes, prostaglandins. The number of basophils increases in the final stage of the inflammatory reaction (with the basophils dilate the vessels, and heparin facilitates the resorption of the inflammatory focus). Agranulocytes. Lymphocytes are subdivided into -
12. Age-related changes in the leukocyte formula of a child. The first and second "crosses" of neutrophils and lymphocytes. The leukocyte formula, like the number of leukocytes, undergoes significant changes during the first years of a person’s life. If during the first hours of a newborn, granulocytes predominate, by the end of the first week after birth, the number of granulocytes is significantly reduced, and the bulk of them are lymphocytes and monocytes. Starting from the second year of life, a gradual increase in the relative and absolute number of granulocytes and a decrease in mononuclear cells, mainly lymphocytes, begins again. The intersection points of the curves of agranulocytes and granulocytes - 5 months and 5 years. In persons aged 14–15 years, the leukocyte formula is practically the same as that of adults. Great importance in assessing leukograms should be given not only the percentage ratio of leukocytes, but also their absolute values (“leukocyte profile” according to Moshkovsky). It is quite clear that a decrease in the absolute number of certain types of white blood cells leads to an apparent increase in the relative number of other forms of white blood cells. Therefore, only the determination of absolute values can indicate actual changes. 13. Platelets, their number, physiological role. Platelets, or blood plates, are formed from the giant cells of the red bone marrow, megakaryocytes. In the bone marrow, megakaryocytes are tightly pressed to the spaces between fibroblasts and endothelial cells, through which their cytoplasm is released outside and serves as material for the formation of platelets. In the bloodstream, platelets have a round or slightly oval shape, their diameter does not exceed 2-3 microns. A platelet does not have a nucleus, but there are a large number of granules (up to 200) of various structures. In contact with the surface, which differs in its properties from the endothelium, the platelet is activated, it spreads and it appears up to 10 notches and shoots, which can be 5-10 times the diameter of the platelet. The presence of these processes is important for stopping bleeding. Normally, the number of platelets in a healthy person is 2-4-1011 / l, or 200-400 thousand in 1 μl. The increase in the number of thrombocytes carries the name "Thrombocytosis" decrease - "Thrombocytopenia". Under natural conditions, the number of platelets is subject to significant fluctuations (their number increases with pain stimulation, physical exertion, stress), but rarely goes beyond the normal range. As a rule, thrombocytopenia is a symptom of pathology and is observed in radiation sickness, congenital and acquired diseases of the blood system. The main purpose of platelets is to participate in the process of hemostasis (see section 6.4). An important role in this reaction belongs to the so-called platelet factors, which are concentrated mainly in the granules and the platelet membrane. Some of them are denoted by the letter P (from the word platelet - plate) and the Arabic numeral (P 1, P 2, etc.). The most important are P 3, or partial (incomplete) thromboplastin, representing a fragment of the cell membrane; P 4, or antiheparin factor; P 5, or platelet fibrinogen; ADP; contractile protein thrombastenin (resembling actomyosin), vasoconstrictor factors - serotonin, adrenaline, norepinephrine, etc. A significant role in hemostasis is given thromboxane A 2 (TxA 2), which is synthesized from arachidonic acid, which is part of cell membranes (including platelets) under the influence of the enzyme thromboxane synthetase. On the surface of platelets are glycoprotein formations that act as receptors. Some of them are “masked” and expressed after platelet activation by stimulating agents - ADP, adrenaline, collagen, micro-fibrils, etc. Platelets are involved in protecting the body from foreign native agents. They possess phagocytic activity, contain IgG, are a source of lysozyme and β -lysins capable of destroying the membrane of some bacteria. In addition, they contain peptide factors that cause the transformation of “null” lymphocytes (0-lymphocytes) into T- and B-lymphocytes. In the process of platelet activation, these compounds are released into the bloodstream and, in the event of vascular injury, protect the body from the entry of pathogenic microorganisms. Thrombocytopoiesis regulators are short-term and long-acting thrombocytopoietins. They are formed in the bone marrow, spleen, liver, and are also part of megakaryocytes and platelets. Short term thrombocytopoietins increase the detachment of blood platelets from megakaryocytes and accelerate their entry into the blood; long-acting thrombocytopoietins promote the transition of the precursors of giant bone marrow cells to mature megakaryocytes. Thrombocytopoietin activity is directly affected by IL-6 and IL-11. 14. Regulation of erythropoiesis, leukopoiesis and thrombopoiesis. Hemopoietins. The continuous loss of blood cells requires their replacement. Formed from non-differentiated stem cells in the red inert brain. Of which arise the so-called colonostimulating (CFU), which are the precursors of all blood lines. Both bi and unipotent cells can arise from them. From them is the differentiation and formation of various forms of red blood cells and white blood cells. 1. Proeritroblast 2. Erythroblast - Basophilic Polychromatic Orthochromatic (loses the nucleus and goes into reticulocyte) 3. The reticulocyte (contains the remains of RNA and ribosomes, the formation of hemoglobin continues) 25-65 * 10 * 9 l in 1-2 days turn into mature erythrocytes. 4. Erythrocyte - every minute 2.5 million mature erythrocytes are formed. Factors Accelerating Erythropoiesis 1. Erythropoietins (formed in the kidneys, 10% in the liver). Accelerate the processes of mitosis, stimulate the transition of reticulocyte to mature forms. 2. Hormones - somatotropic, ACTH, androgenic, hormonal adrenal cortex, inhibit erythropoiesis - estrogens 3. Vitamins - B6, B12 (external blood formation factor, but absorption occurs if it is combined with the internal factor of Castle, which is formed in the stomach), folic acid. You also need iron. The formation of leukocytes is stimulated by leukopoetin substances, which accelerate the maturation of granulocytes and contribute to their release from the red bone marrow. These substances are formed during the breakdown of tissue, in the foci of inflammation, which increases the maturation of leukocytes. There are interleukins, which also stimulate the formation of leuccoites. HGH and adrenal hormones cause leukocytosis (an increase in the number of hormones). Thymosin is necessary for the maturation of T-lymphocytes. In the body there are 2 reserves of leukocytes - vascular - accumulation along the walls of blood vessels and bone marrow reserve in pathological conditions there is a release of leukocytes from the bone marrow (30-50 times more). 15. Blood clotting and his biological significance. The rate of coagulation in an adult and a newborn. Coagulation factors. If the blood released from a blood vessel is left for some time, it first turns into a jelly from a liquid, and then a more or less dense clot is formed in the blood, which, contracting, squeezes out a liquid called blood serum. This is plasma devoid of fibrin. The process described is called blood coagulation. (hemocoagulation). Its essence lies in the fact that protein dissolved in plasma fibrinogen under certain conditions becomes insoluble and precipitates in the form of long fibrin filaments. In the cells of these threads, as in the grid, the cells get stuck and the colloidal state of the blood as a whole changes. The value of this process lies in the fact that coagulated blood does not flow from a wounded vessel, preventing the death of the organism from blood loss. Blood coagulation system. Enzymatic Coagulation Theory. The first theory explaining the process of blood coagulation by the work of special enzymes was developed in 1902 by the Russian scientist Schmidt. He believed that the coagulation proceeds in two phases. In the first one of the plasma proteins prothrombin under the influence of the blood cells released from the injured blood cells, especially platelets, ( thrombokinase) and ca ions goes into an enzyme thrombin. In the second stage, under the influence of the enzyme thrombin, fibrinogen dissolved in the blood becomes insoluble fibrinwhich causes blood to clot. In the last years of his life, Schmidt began to isolate 3 phases in the process of hemocoagulation: 1 - the formation of thrombokinase, 2 - the formation of thrombin. 3- fibrin formation. Further study of the mechanisms of coagulation showed that this view is very schematic and does not fully reflect the whole process. The main reason is that there is no active thrombkinase in the body, i.e. an enzyme capable of converting prothrombin into thrombin (according to the new enzyme nomenclature, this should be called prothrombinase). It turned out that the process of formation of prothrombinase is very complex, a whole series of so-called ones are involved thrombogenic protein enzymes, or thrombogenic factors, which, interacting in a cascade process, are all necessary in order for blood to clot normally. In addition, it was found that the process of coagulation does not end with the formation of fibrin, because at the same time begins its destruction. Thus, the modern blood clotting scheme is much more complicated than Schmidtov. The modern scheme of blood coagulation includes 5 phases, successively replacing each other. The phases are as follows: 1. The formation of prothrombinase. 2. The formation of thrombin. 3. The formation of fibrin. 4. Polymerization of fibrin and clot organization. 5. Fibrinolysis. Over the past 50 years, many substances have been discovered that are involved in blood coagulation, proteins, the absence of which in the body leads to hemophilia (non-clotting). Having considered all these substances, the international conference of hemocoagulologists decided to designate all plasma coagulation factors with Roman numerals, cellular ones with Arabic ones. This was done in order to eliminate confusion in the names. And now, in any country after the commonly accepted name of a factor (they may be different), the number of this factor in the international nomenclature is indicated. In order for us to continue to consider the coagulation scheme, let's first give a brief description of these factors. BUT. Plasma coagulation factors . I. Fibrin and fibrinogen . Fibrin is the end product of a blood coagulation reaction. The coagulation of fibrinogen, which is its biological feature, occurs not only under the influence of a specific enzyme, thrombin, but may be caused by the venom of some snakes, papain, and other chemicals. Plasma contains 2-4 g / l. Place of formation - reticuloendothelial system, liver, bone marrow. Ii. Thrombin and prothrombin . In the circulating blood, only traces of thrombin are normally found. Its molecular weight is half the molecular weight of prothrombin and is equal to 30 thousand. The inactive precursor of thrombin, prothrombin, is always present in the circulating blood. This glycoprotein, which consists of 18 amino acids. Some researchers believe that prothrombin is a complex compound of thrombin and heparin. Whole blood contains 15–20 mg% prothrombin. This content is abundant enough to translate all blood fibrinogen into fibrin. The level of prothrombin in the blood is a relatively constant value. From the moments causing fluctuations of this level, it is necessary to indicate menstruation (increase), acidosis (decreases). Acceptance of 40% alcohol increases the prothrombin content by 65-175% after 0.5-1 hours, which explains the tendency to thrombosis in individuals who regularly consume alcohol. In the body, prothrombin is constantly used and simultaneously synthesized. An important role in its formation in the liver is played by antihemorrhagic vitamin K. It stimulates the activity of liver cells synthesizing prothrombin. Iii.Thromboplastin . In the blood of this factor in the active form is not. It is formed when damage to blood cells and tissues and can be respectively blood, tissue, erythrocyte, platelet. In its structure, it is a phospholipid, similar to the phospholipids of cell membranes. According to the thromboplastic activity, the tissues of various organs descending are arranged in this order: lungs, muscles, heart, kidneys, spleen, brain, liver. Sources of thromboplastin are also breast milk and amniotic fluid. Thromboplastin is involved as an essential component in the first phase of blood coagulation. Iv. Calcium ionized, Ca ++. The role of calcium in the blood clotting process was also known to Schmidt. It was then that he offered sodium citrate as a blood preservative, a solution that bound Ca ++ ions in the blood and prevented its clotting. Calcium is necessary not only for the conversion of prothrombin to thrombin, but for other intermediate stages of hemostasis, in all phases of coagulation. The content of calcium ions in the blood is 9-12 mg%. V and VI.Proaccelerin and Accelerin (AU-Globulin ). Formed in the liver. Participates in the first and second phases of coagulation, while the number of pro-acecerin decreases, and Accelerin increases. Essentially V is the precursor of factor VI. Activated by thrombin and Ca ++. It is an accelerator (accelerator) of many enzymatic coagulation reactions. VII.Proconvertin and convertin . This factor is a protein included in the beta globulin fraction of normal plasma or serum. Activates tissue prothrombinase. Vitamin K is necessary for the synthesis of proconvertin in the liver. The enzyme itself becomes active when in contact with damaged tissues. Viii.Antihemophilic globulin A (AGG-A ). Participates in the formation of blood prothrombinase. Able to provide blood coagulation without contact with tissues. The absence of this protein in the blood is the cause of the development of genetically determined hemophilia. Received now in a dry form and used in the clinic for its treatment. Ix.Antihemophilic globulin B (AGG-B, Christmas factor , the plasma component of thromboplastin). Participates in the process of coagulation as a catalyst, as well as part of the blood thromboplastic complex. Contributes to the activation of the X factor. X.Koller's factor, Steward-Power factor . The biological role is reduced to participation in the formation of prothrombinase, as it is its main component. When clotting is disposed of. Named (like all other factors) by the names of patients in whom a form of hemophilia was first discovered, associated with the absence of this factor in their blood. Xi.Rosenthal factor, plasma thromboplastin precursor (PPT ). Participates as an accelerator in the process of formation of active prothrombinase. Refers to beta blood globulins. Reacts in the first stages of phase 1. It is formed in the liver with the participation of vitamin K. Xii.Contact factor, Hageman factor . Plays the role of a trigger in blood coagulation. Contact of this globulin with a foreign surface (vessel wall roughness, damaged cells, etc.) leads to the activation of the factor and initiates the whole chain of coagulation processes. The factor itself is adsorbed on the damaged surface and does not enter the bloodstream, thereby preventing the generalization of the coagulation process. Under the influence of adrenaline (under stress) is partially able to activate directly in the bloodstream. Xiii.Fibrinstabilizer Lucky-Lorand . Necessary for the formation of finally insoluble fibrin. This is a transpeptidase that stitches individual fibers of fibrin with peptide bonds, contributing to its polymerization. Activated by thrombin and Ca ++. In addition to plasma, there is in uniform elements and tissues. The described 13 factors are generally recognized basic components necessary for the normal process of blood coagulation. The various forms of bleeding caused by their absence relate to different types of hemophilia. B. Cellular Coagulation Factors. Along with plasma factors, the primary role in blood coagulation is played by cellular, released from blood cells. Most of them are contained in platelets, but they are in other cells. It is just that during blood coagulation, platelets are destroyed in greater numbers than, say, erythrocytes or leukocytes, therefore platelet factors are of the greatest importance in coagulation. These include: 1f.Platelet AU Globulin . Similar to V-VI blood factors, performs the same function, accelerating the formation of prothrombinase. 2f.Thrombin Accelerator . Accelerates the action of thrombin. 3f.Thromboplastic or phospolipid factor . It is in granules in an inactive state, and can only be used after the destruction of platelets. Activated upon contact with blood, necessary for the formation of prothrombinase. 4f.Antiheparin factor . Binds heparin and retards its anti-coagulant effect. 5f.Platelet fibrinogen . It is necessary for the aggregation of platelets, their viscous metamorphosis and consolidation of the platelet plug. It is located inside and outside the platelet. contributes to their bonding. 6f.Retractozyme . Provides a blood clot. Several substances are determined in its composition, for example, thrombostenin + ATP + glucose. 7f.Antifibinosilin . It inhibits fibrinolysis. 8f.Serotonin . Vasoconstrictor. The exogenous factor, 90% is synthesized in the gastrointestinal mucosa, the remaining 10% is in platelets and the central nervous system. It is released from the cells when they are destroyed, contributes to the spasm of small vessels, thereby helping to prevent bleeding. In total, up to 14 factors are found in platelets, such as antithromboplastin, fibrinase, plasminogen activator, AC-globulin stabilizer, platelet aggregation factor, etc. In other blood cells, there are basically the same factors, but they do not normally play a noticeable role in hemocoagulation. WITH.Tissue coagulation factors Participate in all phases. These include active thromboplastic factors like plasma factors III, VII, IX, XII, XIII. In the tissues there are activators of the V and VI factors. A lot of heparin, especially in the lungs, prostate gland, kidneys. There are also antiheparin substances. In inflammatory and cancer diseases, their activity increases. There are many activators (kinins) and fibrinolysis inhibitors in the tissues. Especially important are the substances contained in the vascular wall. All these compounds are constantly coming from the walls of blood vessels into the blood and regulate clotting. Tissues also provide removal of coagulation products from blood vessels. 16. Blood coagulation system, blood coagulation factors (plasma and laminar) Factors that support the liquid state of the blood. The function of blood is possible when transporting it through vessels. Damage to the blood vessels could cause bleeding. Blood can perform its functions in a liquid state. Blood can form a blood clot. This will block the blood flow and lead to blockage of blood vessels. Their mortification causes a heart attack, a necrosis-consequence of an intravascular thrombus. For the normal function of the circulatory system, it must have fluid and properties, but if it is damaged, coagulation. Hemostasis is a series of consecutive reactions that stop or reduce bleeding. These reactions include -
The first reaction - compression and contraction - occurs due to the reduction of muscular elements, due to the release of chemicals. Endothelial cells (in the capillaries) stick together and close the lumen. In larger cells with smooth muscle elements depolarization occurs. The tissues themselves can react and squeeze the vessel. The area around the eyes has very weak elements. Very well compressed vessel during childbirth. Vasoconstriction causes - serotonin, adrenaline, fibrinopeptide B, thromboxane A2. This primary reaction improves bleeding. Formation of platelet thrombus (associated with the function of platelets) Platelets are non-nuclear elements, have a flat shape. Diameter - 2-4 microns, thickness - 0.6-1.2 microns, volume 6-9 femtol. The number of 150-400 * 10 in 9 liters. Formed from megakaryocytes by shnirvaniya. Life expectancy is 8-10 days. Electron microscopy of platelets allowed to establish that these cells have a difficult structure, despite their small size. Outside the platelet is covered with a thrombotic membrane with glycoproteins. Glycoproteins form receptors that can interact with each other. The platelet membrane has an indentation that increases the area. In these membranes there are canalici to expel substances from the inside. Phosphomembranes are very important. Laminar factor from membrane phospholipids. Under the membrane there are dense tubes - the remnants of the sarcoplasmic reticulum with calcium. Microtubules and filaments of actin, myosin, which support the form of platelets, are also found under the membrane. Inside the platelets there are mitochondria and dense dark granules and alpha granules - light. Platelets are distinguished by 2 types of pellets containing bodies. In dense - ADP, serotonium, calcium ions Light (alpha) - fibrinogen, von Willebrand factor, plasma factor 5, antiheparin factor, plate factor, beta-thromboglobulin, thrombospondin and plate-like growth factor. The plates also have lysosomes and glycogen granules. When the vessels are damaged, the plates take part in the aggregation processes and the formation of a platelet thrombus. This reaction is due to a number of properties inherent in the plate - When the vessels are damaged, subendothelial proteins are exposed - adhesion (the ability to adhere to these proteins due to receptors on the plate. Adhesion is also promoted by Willebrank factor). In addition to the adhesion properties, platelets have the ability to change their shape and - release active substances (Thromboxane A2, serotonin, ADP, membrane phospholipids - lamella factor 3, thrombin is released - coagulation - thrombin), and aggregation (gluing with each other) is also characteristic. These processes lead to the formation of a platelet thrombus, which is capable of stopping bleeding. The formation of prostaglandins plays an important role in these reactions. From phospholipyl membranes - arachidonic acid is formed (under the action of phospholipase A2), - Prostaglandins 1 and 2 (under the action of cyclooxygenase). For the first time formed in the prostate gland in men. - They are converted to thromboxane A2, which suppresses adenylate cyclase and increases the content of calcium ions - aggregation occurs (gluing of the plate). In the endothelium of the vessels, simply cyclin is formed - it activates adenylate cyclase, reduces calcium, which inhibits aggregation. The use of aspirin - reduces the formation of thromboxane A2, without affecting prostacyclin. The coagulation factors that lead to the formation of a blood clot. The essence of the blood coagulation process is the transformation of soluble plasma protein fibrinogen into insoluble fibrin under the action of thrombin protease. This is the final blood clotting. In order for this to happen, the action of the blood coagulation system is necessary, which includes blood coagulation factors and they are subdivided into plasma (13 factors) and there are laminar factors. In the coagulation system also includes anti-factors. All factors are inactive. In addition to coagulation there is a fibrinolytic system - the dissolution of the formed blood clot. . Plasma coagulation factors - 1. Fibrinogen is a unit of fibrin polymer with a concentration of 3000 mg / l 2. Prothrombin 1000 - Protease 3. Tissue thromboplastin - a cofactor (released when cell damage) 4. Ionized calcium 100 - cofactor 5. Proaccelerin 10 - cofactor (active form - Accelerin) 7. Proconvertin 0.5 - protease 8. Antihemophilic globulin A 0,1 - cofactor. Connected to the Willibring factor 9. Christmas Factor 5 - Protease 10. Stewart-Prowiver 10 Factor - Protease 11. Plasma precursor of thromboplastin (Rosenthal factor) 5 - protease. His absence leads to type C hemophilia. 12. Hageman 40 - protease factor. With it begin the processes of coagulation 13. Fibrin stabilizing factor 10 - transamidase Without numbers Prekallikrein (Fletcher factor) 35 - protease Kininogen with a high MV factor (Fitzgerald factor.) - 80 - cofactor Platelet Phospholipids Among these factors are inhibitors of blood coagulation factors, which prevent the onset of a blood coagulation reaction. Of great importance is the smooth wall of blood vessels, the endothelium of blood vessels is covered with a thin film of heparin, which is an anticoagulant. Inactivation of products that form during blood coagulation is thrombin (10 ml is enough to coagulate all the blood in the body). There are mechanisms in the blood that prevent such action of thrombin. Phagocytic function of the liver and some other organs that are capable of absorbing thromboplastin 9,10 and 11 factors. The decrease in the concentration of blood coagulation factors is carried out by constant blood flow. All this inhibits the formation of thrombin. Already formed thrombin is absorbed by the fibrin filaments, which are formed during blood coagulation (they absorb thrombin). Fibrin is antithrombin 1. Another antitrobin 3 inactivates the resulting thrombin and its activity increases with the combined action of heparin. This complex inactivates 9, 10, 11, 12 factors. The resulting thrombin binds to thrombomodulin (located on endothelium cells). As a result, the thrombomodulin-thrombin complex promotes the conversion of protein C into an active protein (form). Together with protein C, protein S acts. They inactivate 5 and 8 blood coagulation factors. For their formation, these proteins (C and S) require the supply of vitamin K. Through the activation of protein C in the blood, a fibrinolytic system is opened, which is designed to dissolve the thrombus formed and performed its task. The fibrinolytic system includes factors that activate and inhibit this system. In order for the blood to dissolve, activation of plasminogen is necessary. Plasminogen activators are tissue plasminogen activator, which is also in an inactive state and plasminogen can activate 12 active factors, kallikrein, high-molecular kininogen, and urokinase and streptokinase enzymes. To activate tissue plasminogen activator, thrombin needs to interact with thrombomodulin, which are activators of protein C, and activated protein C activates tissue plasminogen activator and it converts plasminogen to plasmin. Plasmin provides lysis of fibrin (makes insoluble filaments soluble) Exercise, emotional factors leads to the activation of plasminogen. During childbirth, sometimes in the uterus, a large amount of thrombin can also be activated, this condition can lead to threatening uterine bleeding. Large amounts of plasmin can act on fibrinogen, reducing its content in plasma. Increased content of plasmin in venous blood, which also contributes to blood flow. In the venous vessels there are conditions for the dissolution of a blood clot. Currently used drugs plasminogen activators. This is important in myocardial infarction, which will prevent the immobilization of the site. In clinical practice, drugs are used that are prescribed to prevent blood clotting - anticoagulants, while anticoagulants are divided into a group of direct action and indirect action. The first group (direct) includes salts of citric and oxalic acids - sodium citrate and ionic sodium, which bind calcium ions. You can restore by adding potassium chloride. Hirudin (leeches) is antithrombin, can inactivate thrombin, therefore leeches are widely used in therapeutic purposes. Heparin is also prescribed as a drug to prevent blood clotting. Heparin is also included in numerous ointments and creams. Indirect anticoagulants include vitamin K antagonists (in particular, drugs derived from clover - Dicoumarin). With the introduction of dicoumarin into the body, the synthesis of vitamin K dependent factors is disturbed (2,7,9,10). In children, when the microflora is underdeveloped blood clotting processes. 17. Stopping bleeding in small vessels. Primary (vascular platelet) hemostasis, its characteristics. Vascular-platelet hemostasis is reduced to the formation of a platelet plug, or a platelet thrombus. Conditionally it is divided into three stages: 1) temporary (primary) vasospasm; 2) formation of platelet plug due to adhesion (attachment to the damaged surface) and aggregation (gluing together) of platelets; 3) retraction (contraction and compaction) of the thrombocytic plug. Immediately after injury occurs primary blood vessel spasm, so that bleeding in the first seconds may not occur or is limited. Primary vasospasm is caused by a release into the blood in response to painful irritation of adrenaline and norepinephrine and lasts no more than 10-15 s. In the next comes secondary spasm, due to the activation of platelets and the release into the blood of vasoconstrictor agents - serotonin, TxA 2, adrenaline, etc. Damage to blood vessels is accompanied by immediate activation of platelets, which is caused by the appearance of high concentrations of ADP (from collapsing red blood cells and injured blood vessels), as well as exposure of the subendothelium, collagen and fibrillar structures. As a result, secondary receptors are “revealed” and optimal conditions are created for adhesion, aggregation and formation of platelet plug. Adhesion is due to the presence in plasma and platelets of a special protein, von Willebrand factor (FW), which has three active centers, two of which are associated with expressed platelet receptors, and one with subendothelial receptors and collagen fibers. Thus, the platelet with the help of FW is “suspended” to the injured surface of the vessel. At the same time as adhesion, platelet aggregation occurs using fibrinogen, a protein found in plasma and platelets and forming binding forces between them, which leads to the appearance of a platelet plug. An important role in adhesion and aggregation is played by a complex of proteins and polypeptides, which are called "integrins". The latter serve as binding agents between individual platelets (when glued to each other) and structures of the damaged vessel. Platelet aggregation may be reversible (following aggregation, disaggregation occurs, i.e. the disintegration of aggregates), which depends on an insufficient dose of the aggregating (activating) agent. From the platelets subjected to adhesion and aggregation, granules and the biologically active compounds contained in them — ADP, adrenaline, norepinephrine, factor P 4, TxA 2, etc. — are strongly secreted (this process is called the release reaction), which leads to a secondary, irreversible aggregation. Simultaneously with the release of platelet factors, the formation of thrombin occurs, drastically increasing aggregation and leading to the appearance of a fibrin network in which individual erythrocytes and leukocytes get stuck. Thanks to the contractile protein thrombosthenin, platelets pull up to each other, the platelet plug is reduced and compacted, i.e. it comes retraction. Normally, stopping bleeding from small vessels takes 2-4 minutes. An important role for vascular-platelet hemostasis is played by arachidonic acid derivatives - prostaglandin I 2 (PgI 2), or prostacyclin, and TxA 2. While preserving the integrity of the endothelial cover, the effect of Pgl predominates over TxA 2, so that in the bloodstream no platelet adhesion or aggregation is observed. When the endothelium is damaged at the site of injury, Pgl synthesis does not occur, and then TxA 2 effect appears, leading to the formation of a platelet plug. 18. Secondary hemostasis, hemocoagulation. Hemocoagulation phases. External and internal ways of activating the process of blood coagulation. The composition of the thrombus. Let us now try to combine all the folding factors into one common system and analyze modern scheme hemostasis. The chain reaction of blood coagulation begins from the moment of contact of the blood with the rough surface of the wounded vessel or tissue. This causes the activation of plasma thromboplastic factors and then the gradual formation of two distinctly different in their properties prothrombinases - blood and tissue .. However, before the chain reaction of prothrombinase formation is completed, processes involving platelets (so-called) occur at the site of damage to the vessel. vascular platelet hemostasis). Due to their ability to adhere, platelets stick to the damaged part of the vessel, stick to each other, gluing together with platelet fibrinogen. All this leads to the formation of so-called. lamellar thrombus ("Gaiema platelet hemostatic nail"). Platelet adhesion occurs due to ADP released from endothelium and red blood cells. This process is activated by wall collagen, serotonin, XIII factor and contact activation products. At first (within 1-2 minutes) the blood still passes through this loose plug, but then something happens. viscose degeneration of a blood clot, it thickens and the bleeding stops. It is clear that such an end of events is possible only if small vessels are wounded, where blood pressure is not able to squeeze this "nail." Coagulation phase 1 . During the first phase of coagulation, education phase prothrombinase, there are two processes that take place at different speeds and have different meanings. This is the process of formation of blood prothrombinase, and the process of formation of tissue prothrombinase. The duration of phase 1 is 3-4 minutes. however, it takes only 3-6 seconds to form tissue prothrombinase. The amount of formed tissue prothrombinase is very small, it is not enough to convert prothrombin to thrombin, but tissue prothrombinase acts as an activator of a number of factors necessary for the rapid formation of blood prothrombinase. In particular, tissue prothrombinase leads to the formation of a small amount of thrombin, which translates into active factors V and VIII factors of the internal level of coagulation. A cascade of reactions ending in the formation of tissue prothrombinase ( external hemocoagulation mechanism), as follows: 1. Contact of destroyed tissues with blood and activation of factor III - thromboplastin. 2. III factor translates VII to VIIa (proconvertin to convertin). 3. The complex is formed (Ca ++ + III + VIIIa) 4. This complex activates a small amount of X factor - X goes to Ha. 5. (Xa + III + Va + Ca) form a complex that has all the properties of tissue prothrombinase. The presence of Va (VI) is due to the fact that there are always traces of thrombin in the blood, which activates V factor. 6. The resulting small amount of tissue prothrombinase converts a small amount of prothrombin to thrombin. 7. Thrombin activates a sufficient amount of V and VIII factors necessary for the formation of blood prothrombinase. If this cascade is turned off (for example, if using caution using paraffinized needles, to take blood from a vein, preventing its contact with tissues and a rough surface, and place it in a waxed tube), the blood coagulates very slowly, within 20-25 minutes and longer. Well, normally, simultaneously with the process already described, another cascade of reactions associated with the action of plasma factors is launched, and ending with the formation of blood prothrombinase in an amount sufficient to translate a large amount of prothrombin from thrombin. These reactions are as follows ( interior hemocoagulation mechanism): 1. Contact with a rough or alien surface leads to the activation of factor XII: XII - XIIa. At the same time, Gaiam's hemostatic nail begins to form. (vascular platelet hemostasis). 2.Active XII factor turns XI into an active state and a new complex is formed. XIIa + Ca ++ + XIa+ III (f3) 3. Under the influence of this complex, factor IX is activated and a complex is formed IXa + Va + Ca ++ + III (f3). 4. Under the influence of this complex, a significant amount of X factor is activated, after which the last complex of factors is formed in large quantities: Xa + Va + Ca ++ + III (f3), which is called blood prothrombinase. Normally, this process takes about 4-5 minutes, after which the coagulation proceeds to the next phase. Coagulation phase 2 - thrombin phase lies in the fact that under the influence of the enzyme prothrombinase II factor (prothrombin) becomes active (IIa). This is a proteolytic process, the prothrombin molecule is split into two halves. The resulting thrombin goes to the implementation of the next phase, and is also used in the blood to activate an increasing amount of Accelerin (V and VI factors). This is an example of a system with positive feedback. The thrombin phase takes a few seconds. 3 phase of coagulation - fibrin formation phase - also an enzymatic process, as a result of which a piece of several amino acids is split off from fibrinogen due to the action of the proteolytic enzyme thrombin, and the residue is called fibrin monomer, which differs sharply from fibrinogen in its properties. In particular, it is capable of polymerization. This compound is referred to as Im. Coagulation phase 4 - polymerization of fibrin and the organization of a clot. She also has several stages. At first, within a few seconds, the formation of long filaments of a fibrin polymer occurs under the influence of blood pH, temperature, and ionic composition of the plasma. Is which, however, is still not very stable, as it is able to dissolve in urea solutions. Therefore, in the next stage under the action of the fibrin stabilizer Laki-Lorand ( XIII factor) there is a final stabilization of fibrin and its transformation into fibrin Ij. It falls out of solution in the form of long threads, which form a net in the blood, in the cells of which the cells get stuck. Blood from a liquid state turns into a jelly-like (clotted). The next stage of this phase is the retraction (compaction) of the clot that lasts for quite a long time (several minutes), which occurs due to the contraction of the fibrin filaments under the effect of retractozyme (thrombosthenin). As a result, the clot becomes dense, the serum is squeezed out of it, and the clot turns into a dense stopper, which closes the vessel - a thrombus. Coagulation phase 5 - fibrinolysis. Although it is not actually associated with the formation of a blood clot, it is considered the last phase of hemocoagulation, since during this phase a blood clot occurs only in the zone where it is really necessary. If the thrombus has completely closed the lumen of the vessel, then during this phase this lumen is restored (occurs thrombus recanalization). In practice, fibrinolysis always occurs in parallel with the formation of fibrin, preventing the generalization of coagulation and restricting the process. The dissolution of fibrin is provided by the proteolytic enzyme plasmin (fibrinolysin) which is contained in the plasma in an inactive state as plasminogen (profibrinolysin). The transition of plasminogen to the active state is carried out by a special activator, which in turn is formed from inactive predecessors ( proactivators) released from tissues, blood vessels, blood cells, especially platelets. Acid and alkaline blood phosphatases, cell trypsin, tissue lysokinases, kinins, medium reaction, factor XII play a large role in the processes of conversion of proactivators and plasminogen activators into the active state. Plasmin breaks down fibrin into individual polypeptides, which are then utilized by the body. Normally, human blood begins to clot after 3-4 minutes after it leaks from the body. After 5-6 minutes, it completely turns into a jelly-like clot. You will learn how to determine bleeding time, blood coagulation rate and prothrombin time in practical exercises. All of them have important clinical significance. 19. Fibrinolytic system of blood, its value. Retraction of a blood clot. Interferes with blood clotting and fibrinolytic blood system. According to modern concepts, it consists of profibrinolizina (plasminogen), proactivator and plasma and tissue systems plasminogen activators. Under the influence of activators, plasminogen passes into plasmin, which dissolves the fibrin clot. Under natural conditions, the fibrinolytic activity of the blood depends on the depot of plasminogen, plasma activator, on the conditions that ensure the activation processes, and on the flow of these substances into the blood. Spontaneous activity of plasminogen in a healthy body is observed in a state of excitement, after an injection of adrenaline, during physical exertion and in conditions associated with shock. Among artificial blockers of blood fibrinolytic activity, gamma aminocaproic acid (GABA) occupies a special place. Normal plasma contains a number of plasmin inhibitors, 10 times more than the level of plasminogen in the blood. The state of hemocoagulation processes and the relative constancy or dynamic equilibrium of coagulation factors and anti-coagulation factors are related to the functional state of the hemocoagulation organs (bone marrow, liver, spleen, lungs, vascular wall). The activity of the latter, and hence the state of the process of hemocoagulation, is regulated by neuro-humoral mechanisms. In blood vessels there are special receptors that perceive the concentration of thrombin and plasmin. These two substances and program the activities of these systems. 20. Anticoagulants of direct and indirect action, primary and secondary. Despite the fact that in the circulating blood there are all factors necessary for the formation of a blood clot, under natural conditions, in the presence of the integrity of the blood vessels, the blood remains liquid. This is due to the presence of anticoagulant substances in the bloodstream, which have received the name of natural anticoagulants, or the fibrinolytic link of the hemostasis system. Natural anticoagulants are divided into primary and secondary. Primary anticoagulants are always present in the circulating blood, secondary - are formed as a result of proteolytic cleavage of blood coagulation factors in the process of formation and dissolution of the fibrin clot. Primary anticoagulants can be divided into three main groups: 1) antithromboplastins - having antithromboplastic and antiprothrombinase action; 2) antithrombins - binding thrombin; 3) inhibitors of self-assembly of fibrin - giving the transition of fibrinogen to fibrin. It should be noted that by reducing the concentration of primary natural anticoagulants, favorable conditions are created for the development of thrombosis and DIC. MAJOR NATURAL ANTICOAGULANTS (according to Barkagan 3.S. and Bishevsky K. M.)
To secondary anticoagulants include “waste” coagulation factors (which have taken part in coagulation) and fibrinogen and fibrin degradation products (PDF), which have potent antiaggregatory and anticoagulant effects, as well as stimulating fibrinolysis. The role of secondary anticoagulants is reduced to the restriction of intravascular coagulation of blood and the spread of thrombus in the vessels. 21. Blood groups, their classification, value in blood transfusion. The doctrine of blood types arose from the needs clinical medicine. When blood was being transfused from animals to humans or from humans to humans, doctors often observed severe complications, sometimes resulting in the death of the recipient (the person to whom blood was transfused). With the discovery of a blood group by a Vienna physician K. Landsteiner (1901), it became clear why in some cases transfusions of blood were successful, and in others they ended tragically for the patient. K. Landsteiner first discovered that the plasma, or serum, of some people is able to agglutinate (glue) the erythrocytes of other people. This phenomenon has received the name isohemagglutination. It is based on the presence of antigens in erythrocytes, called agglutinogens and denoted by the letters A and B, and in plasma - natural antibodies, or agglutinins, referred to as α and β . Agglutination of erythrocytes is observed only if the same name agglutinogen and agglutinin are found: A and α , In and β . It is established that agglutinins, being natural antibodies (AT), have two binding sites, and therefore one molecule of agglututin is capable of forming a bridge between two erythrocytes. At the same time, each of the erythrocytes may, with the participation of agglutinins, contact the neighboring one, due to which a conglomerate (agglutinate) of erythrocytes occurs. In the blood of the same person, there can be no agglutinogens and agglutinins of the same name, because otherwise mass erythrocyte glueing would occur, which is incompatible with life. Only four combinations are possible, under which agglutinogens of the same name and agglutinins or four blood groups are not found: I - αβ , II - Aβ , III - B α , IV - AB. In addition to agglutinins, plasma, or serum, blood is contained hemolysins: there are also two types of them and they are designated, like agglyutinins, by letters α and β . When he meets the same agglutinogen and hemolysin, hemolysis of the erythrocytes occurs. The action of hemolysins occurs at a temperature of 37-40 o WITH. That is why the transfusion of incompatible blood in a person already in 30-40 s. erythrocyte hemolysis occurs. At room temperature, if agglutinogens of the same name and agglutinins occur, agglutination occurs, but hemolysis is not observed. In the plasma of people with II, III, IV blood groups there are antiagglutinogens, which left the erythrocyte and tissues. They are designated, as well as agglutinogens, letters A and B (tab. 6.4). Table 6.4. Serological composition of the main blood groups (AVO system) As can be seen from the table, I blood group does not have agglyutinogens, and therefore according to the international classification it is designated as group 0, II is called A, III - B, IV - AB. To decide on the compatibility of blood groups, the following rule is used: the recipient's environment must be suitable for the life of the erythrocyte donor (the person who donates blood). Such a medium is plasma, therefore, the recipient must take into account the agglutinins and hemolysins in the plasma, and the donor - the agglutinogens contained in the erythrocytes. To resolve the issue of compatibility of blood groups, the test blood is mixed with serum obtained from people with different blood groups (Table 6.5). Table 6.5. Compatibility different groups of blood
Note. “+” - the presence of agglutination (groups are incompatible); "-" - lack of agglutination (groups are compatible. The table shows that agglutination occurs in the case of mixing serum of the first group with erythrocytes of the second, third and fourth groups, serum of the second group with erythrocytes of the third and fourth groups, serum of the third group with erythrocytes of the second and fourth groups. Consequently, the blood of the I group is compatible with all other blood groups, therefore a person with the I blood group is called universal donor. On the other hand, erythrocytes of the IV blood group should not give agglutination reactions when mixed with plasma (serum) of people with any blood group, therefore people with IV blood group are called universal recipients. Why, when deciding on compatibility, do not take into account the agglutinins and hemolysins of the donor? This is because agglutinins and hemolysins during transfusion of small doses of blood (200-300 ml) are diluted in a large volume of plasma (2500-2,800 ml) of the recipient and are bound by its anti-agglutinins, and therefore should not be dangerous for erythrocytes. In everyday practice, a different rule is used to resolve the issue of a blood-bred blood group: single-group blood should be transfused, and only for health reasons, when a person has lost a lot of blood. Only in the case of the absence of one-group blood with great care can a small amount of non-group compatible blood be poured. This is explained by the fact that approximately 10–20% of people have a high concentration of very active agglutinins and hemolysins, which cannot be bound by antiagglutinins even in the case of the transfusion of a small amount of nongroup blood. Post-transfusion complications sometimes occur due to errors in the determination of blood groups. It is established that agglutinogens A and B exist in different variants, differing in their structure and antigenic activity. Most of them received a digital designation (A 1, A, 2, A 3, etc., B 1, B 2, and so on). The greater the serial number of the agglutinogen, the less activity it exhibits. Although varieties of agglutinogens A and B are relatively rare, they may not be detected when determining blood groups, which can lead to incompatible blood transfusion. It should also be borne in mind that the majority of human erythrocytes carry the antigen N. This hypertension is always on the surface of cell membranes in people with blood group 0, and is also present as a hidden determinant on the cells of people with blood groups A, B and AB. H is the antigen from which antigens A and B are formed. In persons with blood group I, the antigen is available to the action of anti-H antibodies, which are quite common in people with blood groups II and IV and relatively rare in people with group III. This circumstance can cause blood transfusion complications during blood transfusion of the 1st group to people with other blood groups. The concentration of agglutinogens on the surface of the erythrocyte membrane is extremely high. Thus, one erythrocyte of blood group A 1 contains, on average, 900,000–1,700,000 antigenic determinants, or receptors, to agglutinins of the same name. With an increase in the serial number of the agglutinogen, the number of such determinants decreases. The erythrocyte of group A 2 has a total of 250,000–260,000 anti-gene determinants, which also explains the lower activity of this agglutinogen. Currently, the AB0 system is often referred to as ABH, and instead of the terms "agglutinogens" and "agglutinins", the terms "antigens" and "antibodies" are used (for example, ABH-antigens and ABH-antibodies). 22. Rhesus factor, its value. K. Landsteiner and A. Wiener (1940) found in the red blood cells monkeys monkeys rhesus hypertension, called them rh factor. Later it turned out that approximately 85% of the white race people also have this hypertension. Such people are called Rh-positive (Rh +). About 15% of people do not have this hypertension and are called Rh-negative (Rh). It is known that the Rh factor is a complex system that includes more than 40 antigens, denoted by numbers, letters and symbols. The most common Rh-type antigens are type D (85%), C (70%), E (30%), and e (80%) - they also have the most pronounced antigenicity. The rhesus system does not normally have the same ag-glutenins, but they can appear if a Rh-negative person is to be transfused with Rh-positive blood. Rh factor is inherited. If a woman is Rh, a man is Rh +, then in 50–100% of cases the fetus will inherit the Rh factor from the father, and then the mother and the fetus will be incompatible with the Rh factor. It was established that during such a pregnancy, the placenta has an increased permeability with respect to the erythrocytes of the fetus. The latter, penetrating into the blood of the mother, lead to the formation of anti-titres (anti-Rhesus-agglutinins). Penetrating into the fetal blood, antibodies cause agglutination and hemolysis of its red blood cells. Severe complications arising from the transfusion of incompatible blood and Rh conflict are caused not only by the formation of red blood cell conglomerates and their hemolysis, but also by the intense intravascular coagulation of blood, since the red blood cells contain a set of factors that cause platelet aggregation and the formation of fibrin clots. At the same time, all organs are affected, but the kidneys are especially badly damaged, as clots clog the “wonderful net” of the glomerulus, preventing the formation of urine, which may be incompatible with life. According to modern concepts, the erythrocyte membrane is considered as a set of the most diverse AHs, of which there are more than 500. Only of these AHs can be made up more than 400 million combinations, or group signs of blood. If we take into account all the other AH occurring in the blood, then the number of combinations will reach 700 billion, that is, significantly more than people on the globe. Of course, not all hypertension are important for clinical practice. However, blood transfusions with relatively rarely occurring hypertension can cause severe blood transfusion complications and even death of the patient. Often during pregnancy there are serious complications, including severe anemia, which can be explained by the incompatibility of blood groups in the systems of the little studied antigens of the mother and fetus. In this case, not only the pregnant woman suffers, but the unborn child is also in trouble. The incompatibility of the mother and fetus in blood groups can cause miscarriages and premature births. Hematologists identify the most important antigenic systems: ABO, Rh, MNSs, P, Lutheran (Lu), Kell-Kellano (Kk), Lewis (Le), Duffy (Fy) and Kid (Jk). These systems of antigens are taken into account in forensic medicine to establish paternity and sometimes in the trans-plantation of organs and tissues. Currently, whole blood transfusions are relatively rare, as they use transfusion of various blood components, i.e. they transfuse what is most needed by the body: plasma or serum, erythrocyte, leukocyte or platelet mass. In this situation, fewer antigens are injected, which reduces the risk of post-transfusion complications. 23. Education, life expectancy and destruction of blood cells, Erythropoiesis ,. leukopoez, thrombocytopoz. Regulation of blood formation. Hematopoiesis (hemopoiesis) is a complex process of formation, development and maturation of the blood formed elements. Hematopoiesis is carried out in special organs of hematopoiesis. Part of the hematopoietic system of the body, which is directly related to the production of red blood cells, is called Eritron. Eritron is not any single organ, but disseminated throughout the hematopoietic tissue of the bone marrow. According to modern concepts, a single hematopoietic maternal cell is a precursor cell (stem cell), from which red blood cells, white blood cells, lymphocytes, and platelets are formed through a series of intermediate stages. Red blood cells are formed intravascularly (inside the vessel) in the sinuses of the red bone marrow. Erythrocytes entering the blood from the bone marrow contain basophilic substance stained with basic dyes. Such cells are called reticulocytes. The content of reticulocytes in the blood of a healthy person is 0.2-1.2%. The life of red blood cells is 100-120 days. Red blood cells are destroyed in the cells of the macrophage system. Leukocytes are formed extravascularly (outside the vessel). At the same time, granulocytes and monocytes mature in the red bone marrow, and lymphocytes in the thymus gland, lymph nodes, tonsils, adenoids, lymphatic formations of the gastrointestinal tract, spleen. Life expectancy of leukocytes is up to 15-20 days. Leukocytes die off in the cells of the macrophage system. Platelets are formed from giant megakaryocyte cells in the red bone marrow and lungs. Like leukocytes, platelets develop outside the vessel. Penetration of platelets into the bloodstream is provided by amoebic mobility and activity of their proteolytic enzymes. The life span of platelets is 2–5 days, and according to some data it is up to 10–11 days. Blood plates are destroyed in the cells of the macrophage system. The formation of blood cells takes place under the control of humoral and neural mechanisms of regulation. The humoral components of the regulation of hemopoiesis, in turn, can be divided into two groups: exogenous and endogenous factors. Exogenous factors include biologically active substances - vitamins of group B, vitamin C, folic acid, and also trace elements: iron, cobalt, copper, manganese. These substances, affecting the enzymatic processes in the blood-forming organs, contribute to the maturation and differentiation of the formed elements, the synthesis of their structural (component) parts. Endogenous factors for the regulation of hematopoiesis include: Castle factor, hematopoietins, erythropoietins, thrombocytopoietins, leukopoetins, some hormones of endocrine glands. Hemopoietins - decomposition products of the form elements (leukocytes, platelets, erythrocytes) have a pronounced stimulating effect on the formation of the blood cells. 24. Lymph, its composition and properties. Formation and movement of lymph. Lymph called the fluid contained in vertebrate animals and humans in lymphatic capillaries and vessels. The lymphatic system begins with lymphatic capillaries, which drain all tissue intercellular spaces. The movement of the lymph is carried out in one direction, towards the large veins. On this way, small capillaries merge into large lymphatic vessels, which gradually, increasing in size, form the right lymphatic and thoracic ducts. Not all lymph flows into the bloodstream through the thoracic duct, as some lymphatic trunks (right lymphatic duct, jugular, subclavian and bronchodiastinal) independently flow into the veins. In the course of the lymphatic vessels are the lymph nodes, after passing through which the lymph is again collected in the lymphatic vessels of several large sizes. In starving people, the lymph has a clear or slightly opalescent liquid. Specific weight is on average 1016, the reaction is alkaline, pH - 9. The chemical composition is close to the composition of plasma, tissue fluid, and other biological fluids (cerebrospinal, synovial), but some differences exist and depend on the permeability of the membranes separating them. The most important difference in the composition of lymph from blood plasma is a lower protein content. The total protein content is on average about half of its content in the blood. During the period of digestion, the concentration of substances absorbed from the intestine in the lymph increases sharply. In the hilus (lymph of the mesenteric vessels), the concentration of fat, to a lesser degree of carbohydrates and slightly proteins, increases sharply. The cellular composition of the lymph is not exactly the same, depending on whether it has gone through one or all of the lymph nodes or has not been in contact with them. Accordingly, peripheral and central (taken from the thoracic duct) lymph are distinguished. Peripheral lymph is much poorer in cellular elements. So, in 2 mm. cc peripheral lymph in a dog contains an average of 550 leukocytes, and in the central - 7800 leukocytes. A person in the central lymph can have up to 20,000 leukocytes in 1 mm.cub. Along with lymphocytes, which make up 88% of the lymph composition a small amount red blood cells, macrophages, eosinophils, neutrophils. The total production of lymphocytes in human lymph nodes is 3 million per 1 kg of mass / hour. Main functions of the lymphatic system very diverse and mainly consist in: The return of protein into the blood from tissue spaces; Participating in the redistribution of fluid in the body; In defensive reactions, both by removing and destroying various bacteria, and by participating in immune reactions; Participating in the transport of nutrients, especially fats. Blood is the most intensely circulating fluid that nourishes organs and tissues with oxygen and nutrients. To find out how tissue fluid and lymph are formed - the other two components of a given human environment - you need to turn to the school biology course. These components form a drainage system, which contributes to the process of resorption (resorption) of organic substances and the further removal of metabolic products into the veins. What is tissue fluid: composition, function and mechanism of formationTissue fluid is called the intermediate medium between the blood and the cells of the body. By chemical structure, it resembles plasma, because the formation of intercellular substance is associated with the process of filtering serum. The blood, passing under high pressure through small capillaries penetrating all tissues, is partially filtered through their thin, elastic walls. Due to this property of the blood, the liquid fraction from the plasma penetrates into the intercellular space, forming a tissue fluid. It washes the cells of all organs and tissues, which allows to transport nutrients to them and remove waste products.
The composition of the lymph and its functionsThe above mechanism of formation of tissue fluid and lymph allows us to conclude that both of them have a common basis, since the second component of the internal environment is derived from the first. In the lymph there is water (95%) and leukocytes, lymphocytes and metabolites - the elements formed as a result of the catabolism of organic compounds. The composition of this connective tissue also contains enzymes and vitamins. The lymph does not have platelets, but contains fibrinogen and other substances that increase blood clotting. The amount of protein in the lymph is about 10 times less than in the blood (about 20 g / l). If the walls of the capillaries are damaged, the number of lymphocytes begins to increase automatically. The main objectives of the lymph are:
Lymph movement: volume and speedAfter the tissue fluid and lymph is formed, about 2 ml of lymph per 1 kg of human weight (180-200 ml) flows into the vessels of the drainage system in an hour. During the day about 2 liters of connective fluid forms in the body of an adult. Through the thoracic lymph flow, it can be pumped in a volume of up to 4 liters. For the circulation of this fluid, smooth muscle cells capable of rhythmically contracting are embedded in the walls of the lymphatic vessels. They move the lymph in a given direction. It is very important for the movement of the connective fluid and the work of the skeletal muscles in the contraction stage. During exercise, the speed of movement of the lymph can increase by 15 times, compared with the same parameter at rest. Knowing how to form tissue fluid and lymph, doctors often advise people who are prone to the appearance of edema, walk more in the open air, do regular exercises, and lead an active lifestyle.
Lymph congestion may be caused by mechanical, dynamic or resorption deficiency:
ConclusionFor those interested in the question of how tissue fluid and lymph is formed, let us briefly repeat that tissue fluid is filtered from the plasma through the walls of the capillaries into the intercellular space. Part of this intermediate medium is returned to the blood, the other - enters the lymphatic vessels, which filter and disinfect it, and then transfer it to the venous bed. In the internal environment of the body, blood, tissue fluid and lymph provide a complex of the most complex adaptive reactions of a person to any effects. Tissue fluid transports molecules between cells and blood. This fluid consists of water and solutes that fall into it, probably from blood plasma. The solubility of dust in water and tissue fluids can be positive and negative. If the dust is not toxic and its action on the fabric is reduced to mechanical irritation, the good solubility of such dust is a favorable factor, contributing to its rapid removal from the lungs. In the case of toxic dust, good solubility is negative factor. Living tissue consists of cells washed by tissue fluid. Cyto-lasma of cells and tissue fluid are electrolytes separated by a poorly conductive cell wall. Such a system has a static and polarized electrical capacity. The retention theory of Baer explains the pathogenesis of a congestive nipple with an increase in intracranial pressure by retaining tissue fluid flowing into the cranial cavity along the optic nerve due to compression at the exit of the optical channel. The result is swelling of the nipple, which is enhanced by venous stasis. According to E.Zh. Tron, this theory is more reliable, although not completely proven. Internal environment of the body - It is a collection of liquids (blood, lymph, tissue fluid), participating in the processes of metabolism and maintaining homeostasis (constancy) of the body. Tissue fluidTissue fluid formed by the transition (filtration) of the liquid part of the blood (plasma) from the tissue capillaries. Location - the gaps between the cells of all tissues. The source of education is blood plasma and cellular waste products. The volume in an adult is 20 liters. Composition: water, nutrients and inorganic substances dissolved in it, oxygen, CO 2, decomposition products released from cells. intermediate medium between blood vessels and body cells; the transfer of oxygen from the blood to the cells, and the carbon dioxide from the cell to the blood. Most of the tissue fluid returns to the bloodstream, penetrating through the endothelium of blood capillaries. The other part, not having time to return to the blood, is collected between the cells of the tissues, where the lymphatic vessels originate. Lymph - It is a liquid connective tissue circulating in the vessels of the lymphatic system. Source of formation: in the intercellular spaces, lymphatic vessels originate from the tissue fluid and penetrate almost all organs, with the exception of bones, hair, skin, and the cornea. During the day, a person produces 2-4 liters of lymph. Lymph flowing from different parts body has a different composition, which is determined by the specific activity of different organs and tissues. Most lymph forms in organs with high permeability of blood capillaries (liver). The amount of lymph per 1 kg of body weight: in the liver - 2 1-36 ml, in the heart - 5-18, in the spleen - 3-12, in the muscles of the limbs - 2-3 ml. There are no or few red blood cells in the lymph, there is a small number of leukocytes: neutrophils, eosinophils, basophils. In lymphatic vessels, it is enriched with lymphocytes, which are formed there. Composition of lymphComposition: water with waste products dissolved in it (decomposition of organic substances), proteins - 1-2%, lymphocytes, leukocytes. The composition of the lymph differs from the tissue fluid higher protein content (2 g%). The chemical composition of the lymph is also close to the composition of blood plasma, but it contains less (3-4 times) of proteins, so the lymph has a low viscosity. The composition of the lymph differs from the capillary filtrate and blood plasma. It contains (µg / 100 ml) anions: Cl - - 438, HCO3 - - 48.0, H2PO4 - - 1.5; cations: Na + -524, K + - 9.8, Ca 2+ - 4.5, as well as various enzymes. Lymphatic tissue deposits vitamins. In the lymph are also substances that contribute to more rapid blood clotting. The concentration of the remaining substances corresponds to their content in the blood plasma. Lymph contains fibrinogen, it is able to clot, but much slower than blood. When blood capillaries are damaged, the number of lymphocytes in the lymph increases. In addition to lymphocytes, there are a small number of monocytes and granulocytes in the lymph. There are no blood plates in the lymph, but it coagulates, as it contains fibrinogen and a number of clotting factors. After coagulation of the lymph, a loose, yellowish clot forms and a liquid, called serum, acts. Factors of humoral immunity - complement, properdin, lysozyme were found in the lymph and blood. Their number and bactericidal activity in the lymph is significantly lower than in the blood. In general, lymph is a clear, yellow liquid consisting of water (95.7 ... 96.3%) and dry residue (3.7 ... 4.3%): organic substances - proteins (albumin, globulins, fibrinogen), glucose, lipids, etc., as well as minerals. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Read: |
|---|
New
- Sequence of procedures
- The program of intensive moisturizing of the skin on cosmetics bark
- What you need for acrylic powder
- What does owl mascot mean
- Analyzes for pancreatitis: what research should be done and what indicators show
- Owl - a talisman to attract money and good luck
- What bird screams at night with a kitten's voice?
- Cholesterol and stress
- Manicure at home
- Effective facial