Site sections
Editor's Choice:
- Available methods for rapidly increasing blood leukocytes
- Nail and skin fungus will not resist the coffee grounds
- Crocus furniture exhibition. Furniture exhibitions
- Owl tattoo on arm value
- The biggest members in the world
- Fractures of the phalanges of the toes of the photo
- What is “bad” and “good” cholesterol
- What to do if the skin around the nails dries
- The safest natural varnishes list
- Olive oil: is there any point in buying expensive varieties?
Advertising
| Fracture of the middle toe. Fractures of the phalanges of the toes of the photo |
What is a fracture of the phalanges of the toesSuch fractures occur quite often. This is due to the fact that the phalanges of the fingers are less protected from external influences. Most often, fractures are caused by direct trauma and relatively rarely by indirect. Distal phalanges of the I and II fingers are most often subjected to fractures. These fingers, compared with the others, are much more prominent. Complete fractures of the phalanx can be transverse, oblique, T-shaped or comminuted. Rarely observed tears of the epiphysis of the distal phalanx of the thumb. Comminuted fracture of the proximal phalanx is relatively common. Symptoms of fractures of the phalanges of the toesIn case of fractures of the phalanges of the toes during the first hours after injury, significant swelling, pain at the level of the fracture during palpation, as well as axial load on the injured finger and passive movements of the finger are determined; bruising is determined on the lateral and back surfaces, less often on the plantar side. Displacement of fragments with closed fractures of the phalanges of the toes in most cases does not happen. Sometimes the extensor thrust leads to an angular displacement of fragments, an angle open to the rear. Especially sharply offset is expressed on the proximal phalanx of the thumb. Pain and limp hold on for a long time. To reduce pain, the patient usually carries a support on the heel. Very often, a fracture that seemed closed at the time of injury is complicated, since the skin above the fracture site is also damaged and necrotized. Nail bed often damaged and is the site of infection. Diagnosis of fractures of the phalanges of the toesFractures of the phalanges of the toes are examined radiographically in the frontal and lateral projections. To clarify the displacement of fragments, a snapshot is made in the half-sided projection (in oblique). Many doctors miss sesamoid bone fractures. Fractures of such bones, especially a fracture of the first finger, can only be recognized radiologically. There are observed fatigue fractures of the sesamoid bone of the first finger. Sometimes it is possible to recognize a fracture of a sesamoid bone with certainty only after the development of a callus. Often, a false joint is formed. It is believed that the sesamoid bone acquires a lobular structure as a result of the development of the perestroika process in it in the form of fatigue fractures. In differential diagnosis when reading radiographs, one should be aware of the congenital expansion of sesamoid bones in the area I of the metatarsophalangeal articulation (bipartial, triparial), which in half of cases are bilateral. In contrast to fractures, the extra bones have a rounded shape and clear contours. Fractures of the sesamoid bone are characterized by the serrated surface of the fragments. Treatment of phalanx fractures of the toesAs a rule, patients with fractures of the phalanges of the toes are treated on an outpatient basis. The duration of temporary disability is small. At fracture of the phalanges of the fingers without displacement, a sticky patch is applied in several layers to the corresponding finger. The ability to work with this method of treatment is restored after 2 weeks. It should be considered wrong to leave such fractures without any immobilization. Immobilization with the help of a plaster splint is excessive, cumbersome, in some cases the splash increases pain and increases the duration of disability. The use of a sticky patch allows you to begin active movements in the joints of the injured finger from the first days after the injury, which has a positive effect on its function in the future. Usually on the 2-3rd day, the bandage may weaken, and then it is again supported with a sticky plaster. In case of multiple fractures, immobilization is carried out with a plaster cast in the form of a “shoe” for a period of 2-3 weeks. In case of a fracture of the proximal phalanx of the first finger, plaster immobilization lasts up to 4 weeks. Treatment of fractures of the phalanges of the toes with displacement of fragments presents no particular difficulties. Eliminate displacement most often by stretching along the axis of the damaged finger. The best results are ensured by the use of skeletal traction for this purpose using the Circass-Zadeh tire. With a large displacement of fragments, skeletal traction is imposed after manual reposition, with the help of which they strive to achieve the correct standing of fragments. The traction is continued until the formation of primary callus (10-15 days). Further impose plaster cast in the form of "shoes" to complete healing of the fracture. Open reposition of fragments with fixation by a thin rod of Bogdanov or a Kirchner spoke is shown when it is impossible to eliminate the displacement of fragments in a conservative way. The average duration of disability for fractures of the phalanges of the toes with displacement of fragments is 3-4 weeks. Which doctors should be consulted if you have phalanx fractures of the toes
Promotions and special offersMedical news14.08.2017 From August 15 to September 15, 2017, a special price for tests for schools and kindergartens is valid in the Madis clinic network. 18.04.2017 Scientists from the University of North Carolina found that the immunodeficiency virus can be found not only in blood cells (T cells), but also in other tissues of the body. Experts have determined that the virus can be located inside the so-called macrophages (ameba-like cells). 13.04.2017 The Ministry of Health of the Russian Federation approved the drug Revolide (Eltrombopag) for use in children. New drug It is shown to patients suffering from chronic immune thrombocytopenia (idiopathic thrombocytopenic purpura, ITP), a rare blood system disease. Sarcomas make up almost 5% of all malignant tumors. They are characterized by high aggressiveness, rapid spread by hematogenous route and a tendency to relapse after treatment. Some sarcomas develop over the years, not showing anything ... Viruses not only hover in the air, but can also fall on handrails, seats and other surfaces, while maintaining their activity. Therefore, on trips or public places it is desirable not only to exclude communication with other people, but also to avoid ... Returning good vision and saying goodbye to glasses and contact lenses forever is the dream of many people. Now it can be made reality quickly and safely. New features of laser vision correction opens completely Femto-LASIK contactless technique. Cosmetic preparationsdesigned to care for our skin and hair may not actually be as safe as we think. More than half of the foot bones are represented by the phalanges of the fingers, and, although these bones are very small, if they are damaged, there may be considerable difficulty in walking and serious complications due to late or improper treatment. This kind of foot injury is not uncommon, because the fingers are little protected from damaging external influences. Damage may be caused by impacts, heavy objects falling on the legs, excessive loads. There are also pathological fractures - they are caused by some diseases that lead to a significant decrease in strength. bone tissue. For example, it happens in osteoporosis, tumors, osteomyelitis, hyperparathyroidism. The most frequent are fractures of the thumb and second toe. Also, so-called fatigue fractures of the sesamoid bone of the first finger often occur. Clinical manifestationThe main symptoms of finger fractures are often similar to the signs of other types of injury at this location. It can be difficult to determine its presence or to distinguish it from a bruise, but you should always quickly make an accurate diagnosis for timely appointment. effective treatment. Symptoms of toe fractures are similar to signs of fractures from other sites. The degree of reliability allocate relative and absolute symptoms. Relative allow us to make the assumption that the finger is broken, and the absolute are reliable signs of fracture.
Relative symptoms
Absolute symptoms
When closed-type fractures are formed, fragmental displacement is usually not observed. Sometimes the extension muscles lead to an angular displacement of the fragments. The most often observed displacement, if there is a fracture of the big toe in its proximal phalanx. If the bone grows together in this position, the painfulness when walking remains for a long time. To alleviate the pain, the patient tends to step on the heel. Very often, a closed fracture becomes an open one if purulent-necrotic complications develop at the site of the injury. Often there are damage to the nail bed, which can become the gate of infection. With a toe fracture, the clinical picture is not always clear, especially if the toe is broken without displacing the fragments or there is only a small crack. In such cases, the patient often ignores the symptoms and is unaware of the presence of a fracture. Therefore, in case of any injury of the foot, it is necessary to consult a doctor as soon as possible in order to avoid possible complications. Diagnostics
Reliable diagnosis and accurate localization of phalangeal damage can be established only by X-ray in two projections. Sometimes you have to take a picture in an oblique projection. This study allows you to make an accurate diagnosis with an accuracy of 99%. Radiography in two projections allows the doctor to determine exactly which finger is broken, the localization of the defect and the location of the bone fragments, which allows the doctor to decide on the treatment tactics. It can be difficult to recognize sesamoid (additional) bone fractures. Their presence can be set only radiographically. Sometimes damage to the sesamoid bone can only be found after the formation of callus. ComplicationsA toe fracture can lead to serious consequences even in cases where the injury itself was relatively minor. Some people who have been injured do not rush to seek medical help, since they do not consider the damage significant or do not suspect that the finger is broken, and as a result, they lose time in the hope of a successful self-healing. Sometimes recovery is successful, and sometimes complications bring more inconvenience than the injury itself. There are early and delayed complications. Early include: open fractures, hematoma. Late complications: chronic pain, arthritis, osteomyelitis, ankylosis (limited mobility), finger deformity, false joint (non-union), callus. A timely and accurate diagnosis will allow the doctor to prescribe the right treatment as soon as possible, which will prevent dangerous consequencesseemingly minor but serious injury. Treatment
If there is a suspicion that the finger is broken, it is necessary to immediately consult a doctor or call an ambulance. To reduce pain and swelling, you can apply cold to the injury site. Immobilizing dressings should not be made on their own, as it is possible to cause additional trauma or to cause displacement of fragments. As a rule, patients with such injuries are treated on an outpatient basis by a surgeon. The tactics of treatment depends on which finger is broken, in which phalanx, the type of fracture, the presence of complications and other circumstances. If there are complications, surgery is necessary. Sometimes it is shown reposition and skeletal traction. Immobilization is always recommended. Her method depends on the severity and location of the fracture: it may be a bandage made from adhesive tape, a plaster splint or a plaster cast as a “shoe”. The duration of the plaster immobilization is closely related to the severity of the damage and the presence of complications during the regeneration period. Temporary disability can last from two to four weeks. Fracture Recovery - Basic Techniques For the fastest healing and the best restoration of function, after the removal of the plaster bandage, physiotherapeutic procedures and therapeutic exercises are prescribed. Symptoms of a fracture of a finger Fractures of a phalanx of a finger
... degrees of comminuted fractures of the diaphysis of 2-5 metatarsal bones, fracture of the proximal phalanx of 5 fingers, rupture of the extensor tendon 4 fingers of the right foot. ... degrees of comminuted fractures of the diaphysis of 2-5 metatarsal bones, fracture of the proximal phalanx of 5 fingers, rupture of the extensor tendon 4 fingers of the right foot.
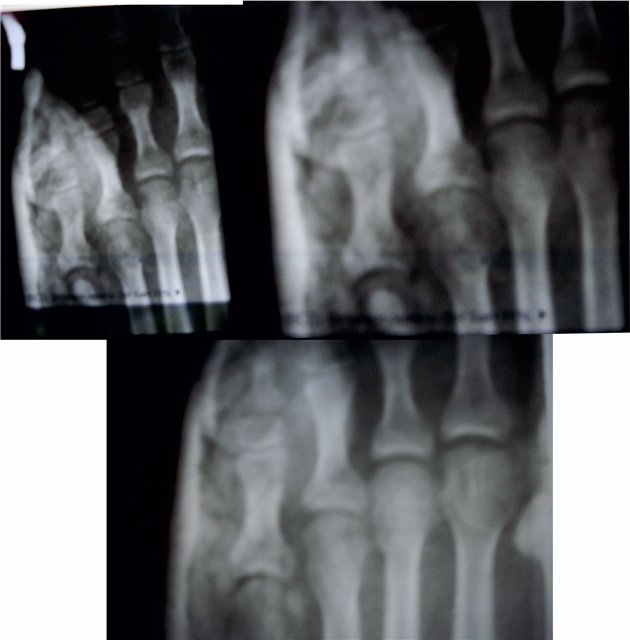
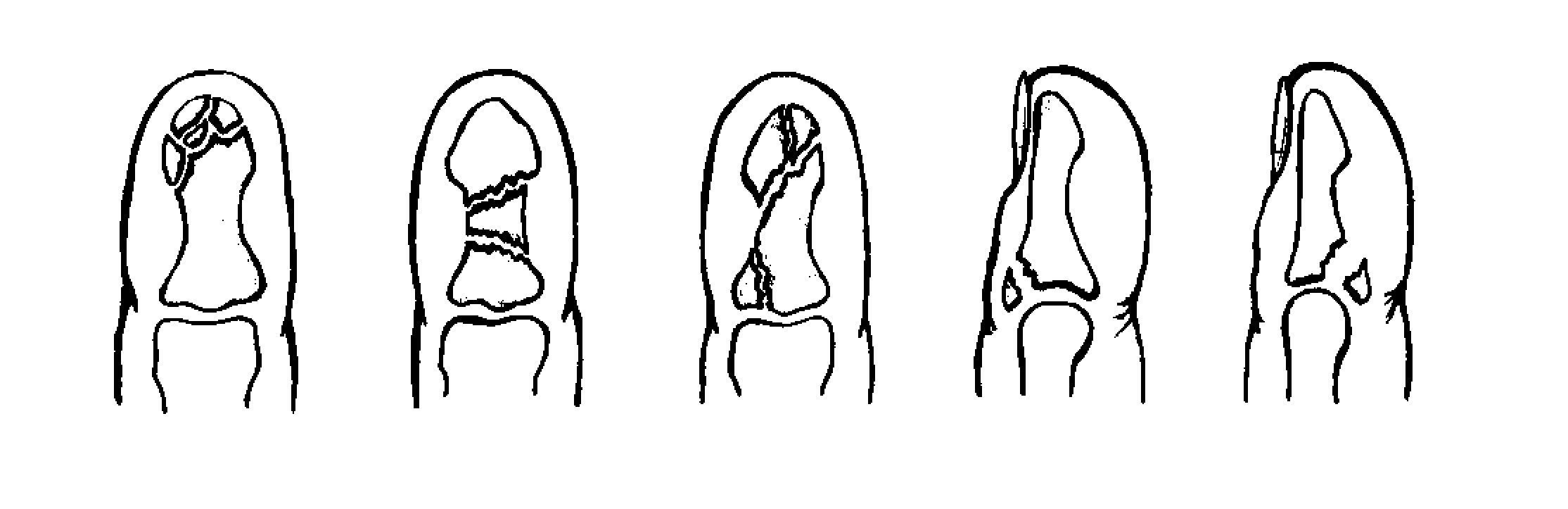
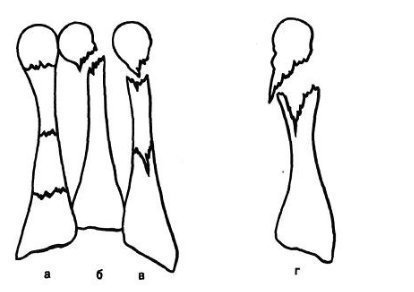
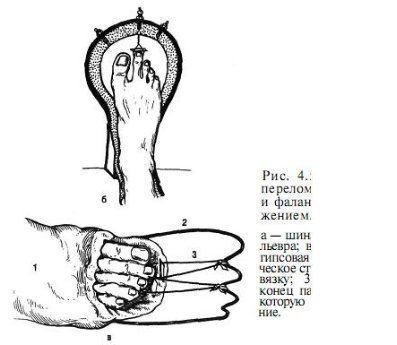
Fractures and fractures of the forefoot according to data from different sources, they constitute from 27.6 to 62.6% of all damages of this localization. These include fractures of the phalanges of the fingers and fractures of the metatarsal bones. Fractures of the phalanges of the toes occur quite often, because, being the end section of the foot, the fingers are least protected from external influences. Most often such injuries occur in direct injury, less often in indirect injuries (falling from a height, hitting a fixed heavy object with a foot, etc.). Indirect injury mechanism occurs mainly in athletes. Distal phalanxes of the I and II toes, which are much more prominent and least protected, are most susceptible to fractures. The injuries of the phalanges of the fingers are distinguished by a great variety - from a simple fracture to comminuted fractures (Fig. 4.1). In case of incomplete (partial) fractures of the phalanges, a piece of bone tissue often occurs in the form of a small wedge in the region of the proximal or distal phalanx. The separation of two fragments of one phalanx at the same time is possible. Complete fractures of the phalanx can be transverse, oblique, T-shaped and comminuted. The epiphysis of the distal phalanx of the thumb is less common. A comminuted fracture of the proximal phalanx is quite common. Clinical picture In case of fractures of the phalanges of the toes during the first hours after injury, significant swelling, pain at the level of the fracture during palpation, as well as axial load on the injured finger and during its passive movements, bruising on the lateral and dorsal surfaces, less often on the plantar side are determined. The displacement of fragments with closed fractures of the phalanges of the toes in most cases does not happen, but sometimes the extensor pull leads to an angular displacement of fragments from the angle open to the rear. Fig. 4.1. Types of fractures of the phalanges of the toes.
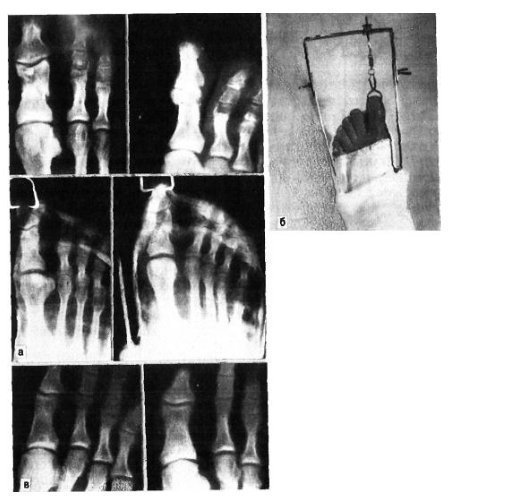
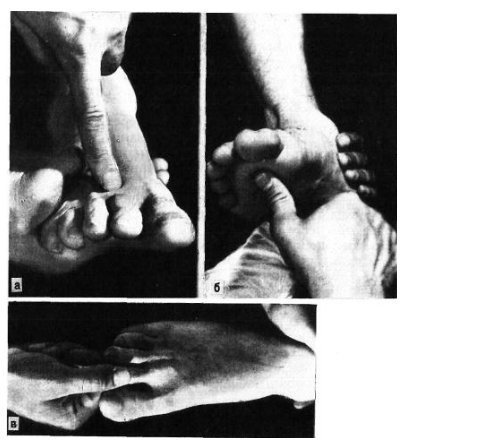
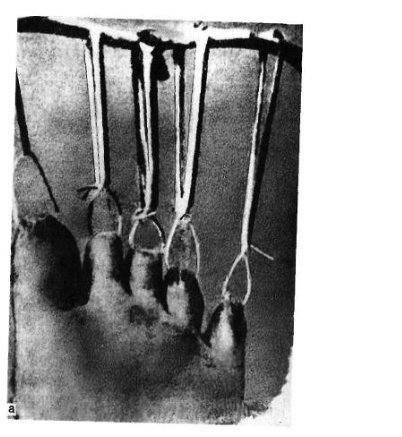
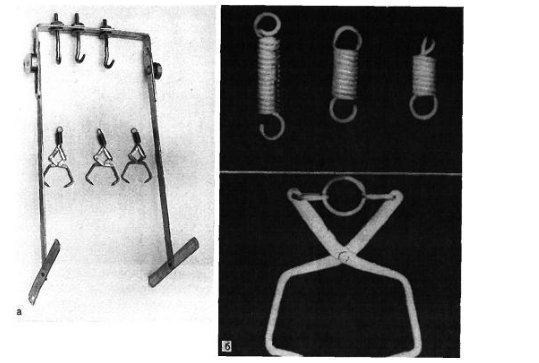
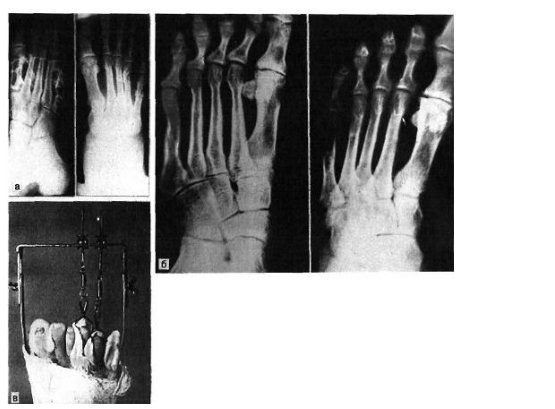
Especially sharply offset is expressed on the proximal phalanx of the thumb. If the fracture grows together in this position, i.e. with angular displacement, pain and lameness remain for a long time. Sparing the foot, the patient usually transfers the support to the heel. It must be emphasized that very often a fracture that seemed to be closed at the time of injury is complicated, since the skin above the fracture site is also damaged and necrotized. The nail bed is often damaged and can be the gateway to the infection. Radiodiagnosis X-ray examination for fractures of the phalanges of the toes is carried out in frontal and lateral projections. To clarify the direction and degree of displacement of fragments resorted to the semi-lateral (oblique) projection. Many doctors still do not suspect the possibility of breaking sesamoid bones. These fractures, and especially the thumb, can only be recognized radiologically. In addition to the usual radiographs in two projections, special stacking of the foot according to Zedgenidze is needed to detect sesamoid bone fractures: the pictures are taken from the plantar side in the position of the patient lying on his stomach. Sometimes it is possible to recognize a fracture of a sesamoid bone only after the appearance of a callus, however it does not always form and in these cases a false joint is formed. In other words, in some cases, a fracture of a sesamoid bone may remain unrecognized. In differential diagnosis, analyzing radiographs, one should be aware of the possibility of congenital cleavage of sesamoid bones in the area of the first metatarsophalangeal joint, and in half of cases it is bilateral (bipartial, tripartial splitting). Intact accessory bones have a rounded shape and clear contours. Fractures of sesamoid bones are characterized by serrated surface of fragments. Treatment Fractures of the phalanges of the toes are usually treated in polyclinic conditions, the duration of temporary disability with them is small. We recommend treatment of fractures of the distal phalanges without displacement as follows. AT soft tissue distal phalanges injected 2-3 ml of 2% solution of novocaine. This removes the pain, and allows you to perform further manipulations. If there is subungal hemorrhage (and this is quite common), you should stupidly move the nail shaft proximally and empty the hematoma. Then the damaged phalanx is treated with an alcoholic solution of iodine and bandaged with adhesive tape in several layers. This is enough to immobilize the damaged phalanx. Immobilization with plaster Longuet here is unnecessary, cumbersome, and sometimes increases the pain and increases the duration of disability. The use of adhesive plaster allows you to start active movements in the joint of the injured finger from the first days, which favorably affects its functions. On the 2-3rd day, the weakened bandage is fixed with adhesive tape. In case of fractures of the middle and proximal phalanges of the fingers (except for the thumb) without displacement or with a slight displacement of fragments, immobilization is also carried out with adhesive tape. Immobilization in case of multiple fractures is carried out with a plaster cast in the form of a “shoe” for 2-3 weeks. At the turn of the proximal phalanx of the thumb, plaster immobilization is continued for up to 4 weeks. Treatment of fractures of the phalanges of the toes with displacement of fragments presents no particular difficulties. To eliminate the displacement, they most often resort to axially extending the damaged finger. The best results are ensured by the use of skeletal traction on the tire of our design for this purpose (Cherkes-Zade tire). With a large displacement of fragments, skeletal traction is imposed after manual reposition, with the help of which the fragments of standing can be properly positioned. Traction continued until the formation of primary bone spur (10-15 days). In the future, impose a plaster cast in the form of "shoes" to complete healing of the fracture. We give the observation. The open reposition of fragments with fixation by a thin Bogdanov rod or a Kirchner spoke is shown when it is impossible to eliminate the displacement of fragments in a conservative manner. The average duration of disability for fractures of the phalanges of the toes with the displacement of fragments 3-4 weeks. Fractures of the metatarsal bones make up 2.3% of skeletal bone fractures and 27.8–45% of foot bone fractures, are isolated, multiple, and can be combined with fractures of other foot bones, often phalanges of the fingers. There are fractures of the base, diaphysis and cervical metatarsal bones. The fracture line can be oblique, transverse, wedge-shaped, etc. (Fig. 4.3). In most cases, fractures result from a direct injury: the fall of a heavy object on the front of the foot, the falling of the foot under the wheel of a moving vehicle. There are cases of an indirect mechanism of injury (a fall from a height, a sharp tucking of the foot). Fracture of the metatarsal bones occurs when the force developed by a traumatic object when falling on a foot exceeds the amount of resistance of the metatarsal bones. The nature of the fracture and the number of broken metatarsal bones depend on the mass of the traumatic object, the speed and direction of its action on a particular section of the foot. With significant mass and speed, a fracture occurs according to the shear mechanism with fragments displaced in width, with smaller masses and speeds - a fracture along the bend mechanism, at which the fragments displacement is insignificant or absent. Fracture of the metatarsal bones by the type of flattening is quite rare. It occurs when the action of the traumatic force falls on the supporting surface of the bone. The mechanism of injury in these cases is crushing bones. The nature of the fractures of the metatarsal bones of the foot in indirect injury depends on its mechanism: flexion, detachment, wedging, twisting. In most cases, the traumatic force is the severity of one’s own body. If the support falls on the back of the foot, there is a fracture of the bones of the back section - heel and talus. If, in the event of a fall, the foot is in the position of the plantar flexion, a fracture of the metatarsal bones occurs. The violation of their integrity occurs at the moment when the fingers and heads of the metatarsal bones hit the support, and the body continues to move by inertia. In such cases, fractures of the metatarsal bones can occur at any level. The fracture mechanism is flexion. It should also be noted that the foot at the time of the fall, as a rule, has a tendency to bend, therefore fractures in the Lisfranc joint often occur, especially diverging ones. Apparently, this is also the mechanism of injury at fractures of the bases of the metatarsal bones. We have 181 observations of the fracture of the metatarsal bones. Fracture from direct violence was obtained in 58.5%, from indirect - in 41.5% of cases. According to our data, the localization of the metatarsal bone fractures depends on the mechanism of injury. With a direct mechanism, I, III, and IV metatarsal bones are more often fractured, while indirect fractures are more often indirect, with IV and V metatarsal bones. Fractures of the base of the metatarsal bones with the indirect mechanism of injury were more frequent than with the direct mechanism, respectively in 30.7 and 17.9% of cases. Diaphyseal fractures of these bones appeared much more often with direct injury than with indirect (respectively 45.3 and 29.3%). The typical localization of a fracture of the V metatarsus is its base. Such a fracture occurs very often and is the result of a sharp contraction of the short fibular muscle tendon attached to the base of the bone. These fractures are often diagnosed as stretching. In all cases, from the anamnesis, they find out whether the injured foot had tucked when falling from a greater or lesser height, when leaving the vehicle, on the stairs. It should be noted that a fracture of the base of the V metatarsus may also occur as a result of direct injury. The direct injury mechanism is possible with supination and turning the foot inward. Sometimes this fracture is combined with a fracture of the lateral ankle. We should not forget about the variant of its individual development, which can be observed in adults and is often interpreted as a fracture. Fracture of the V metatarsal bone, as well as I, can be both isolated and combined with fractures of other bones of the foot. Clinical picture The clinical picture of fresh fractures of the metatarsal bones is not always typical and depends on the nature of the injury, the location of the fracture, the number of broken bones, the presence or absence of significant displacement of fragments. A fracture of one metatarsal gives a very different clinical picture depending on which metatarsal bone is broken. The usual symptoms are deformity and crepitus; mobility of bone fragments is rarely determined. The magnitude of the edema in fractures of the metatarsal bones also depends on the severity of the damage and the number of broken bones. A relatively minor injury and a fracture of the I or II metatarsal bones manifest mild swelling, more on the back of the foot. At the fracture of the base of the V metatarsal bone, there is a limited swelling on the back-outer surface of the foot above the fracture site, often swelling spreads to the external surface of the ankle joint. Hemorrhages in cases of fractures of the metatarsal bones are quite common and are localized, as a rule, on the lateral sides of the foot. Their size depends on the severity and extent of damage to soft tissues and bones. Fracture of the metatarsal bones is often manifested by local pain in the area of the fracture. There is pain and neighboring bones, mainly due to soft tissue injury. To clarify the localization of pain, the doctor gently palpates with the index finger all the metatarsal bones (Fig. 4.4, a). Pressing from the plantar side onto the head of a broken bone, you can cause a symptom of reflected pain according to Jacobson (Fig. 4.4,6). The pain at the fracture site is marked by stifling the injured finger. The symptom of the reflected pain is detected at the fracture site and when the head of the metatarsus of the corresponding finger is pushed (push symptom). However, if this symptom is identified incorrectly, signs of a fracture of the metatarsal bones may not be detected. So, when tapping on the distal phalanxes of the fingers, pain in the place of the fracture may not be observed, because the toes of the foot are easily bent or deflected to the sides and the impulse is not transmitted to the metatarsal bones (exception thumb). In order to detect pain with this symptom, it is necessary to capture the entire finger and push the head of the metatarsal bone (Fig. 4.4, c). At the fracture of one metatarsal bone without pronounced displacement, patients themselves can come to the reception, stepping on the heel, on the outer or inner edge of the foot. The load on a particular department of the foot depends on whether the metatarsal bone is broken - from the outside or the inside. With multiple fractures of the metatarsal bones with a significant displacement of fragments, there is a pronounced dysfunction of the foot, especially the supporting bone, and an attempt to step on even on the heel causes sharp pain. Movement in the ankle joint is also limited due to reflected pain. Fracture of one or two metatarsal bones does not lead to deformity of the foot. This can be explained by the fact that the remaining intact metatarsal bones act as immobilizing dies. Edema in cases of fractures of the metatarsal bones can sometimes obscure the displacement of fragments that sometimes exists. For the same reason, it is not always possible to detect the pathological mobility of bone fragments. Gentle crepitus of fragments in case of fractures of the metatarsal bones is often detected when examining the end of a finger, but it is not always possible to re-obtain it with the same manipulation, since after the first examination fragments often shift. Carefully collected history clarifies the issue of the mechanism of injury and the possibility of fracture. However, on the basis of a clinical trial it is not always possible to establish a diagnosis, therefore, radiography is necessary. Radiodiagnosis Radiographs of the metatarsal bones are performed in straight, lateral and semi-lateral projections. In some cases, a fracture of the metatarsal bone can be identified only with repeated radiography and special laying of the foot. Often on radiographs obtained in the first hours after injury, it is impossible to see a fracture, and only after 2 weeks, and sometimes 3-4 weeks, with repeated X-rays, the gap between the fragments becomes wide and clearly visible due to resorption of the edges of bone fragments. The fracture line and cracks can be located at different levels of the bone and have a different direction. In one of our patients, on the radiograph, the fracture line was not traced at all. Only 2 weeks later, a fracture was found in the picture, the line of which was extended and there were signs of primary callus. The analysis of X-ray diagnostic tests convinces that a single X-ray examination in case of an injury to the forefoot is not always sufficient for establishing a diagnosis. It is necessary to take into account the clinical symptoms and, if there is a suspicion of a fracture, resort to re-x-ray after 2 weeks. Radiological diagnosis of fractures of the base of the metatarsal bones, especially III and IV, is of considerable difficulty without significant displacement of fragments. Difficulties due to the fact that the image of the foot, made in the rear-plantar direction, there is the imposition of shadows of the bases. When conducting differential diagnostics, one should remember about the possibility of the presence of additional bones on radiographs and not treat them as signs of a fracture. Treatment Fractures of the metatarsal bones without displacement or with a slight displacement of fragments are treated by unloading the limb with fixing it with a deep plaster cast to the knee joint in the form of a boot. In case of multiple fractures of the metatarsal bones, we insert a metal instep of our own design into the plantar part of this dressing. The timing of fixation in a plaster cast depends on the number of broken bones, the location and nature of the fracture and averages 3-5 weeks. After removing the plaster bandage, physical therapy, massage, swimming in the pool are prescribed. Dosed load is allowed on the 3rd week at the fracture of one or two metatarsal bones and on the 4th week in case of multiple fractures. In the first days after removing the plaster cast, it is recommended to tightly tape the foot and put an insole in the shoes, and sometimes use orthopedic shoes. Great difficulties arise in the treatment of fractures of the metatarsal bones with displaced fragments. A prerequisite in such cases is a careful comparison of fragments. The remaining unresolved displacement, especially significant, causes pain, swelling, deformity of the foot, violation of statics. Most in a simple way reposition of fragments in case of fractures of the metatarsal bones with an offset is to correct them by manual thrust along the axis behind the fingers with simultaneous pressure on the fragments in the direction opposite to the displacement. The manual reposition technique is as follows. After careful treatment of the damaged foot with warm water and soap of the patient is placed on the table on the back, anesthesia is performed (administration of 10 ml of a 1% solution of novocaine to the fracture site). With insufficient anesthesia, it is not necessary to count on a successful reduction. For the convenience of replenishing the fragments, the leg is bent in knee joint to a right angle so that the heel rests against the edge of the table. The surgeon with one hand produces a pull along the length of the corresponding finger. The assistant for the ankle joint and the lower third of the leg. After 1-2 minutes, when it can be assumed that the fragments are stretched, the surgeon with the finger of the second hand exerts pressure on the displaced distal fragment from the back or plantar surface (depending on which way they are shifted) or in the direction opposite to the displacement. If the surgeon needs to manipulate on the fragments with the fingers of both hands during reposition, a second assistant is needed to stretch the fragments. To improve the efficiency of manual reposition, we recommend that you wear loops from the bandages on the toes of the feet corresponding to the broken metatarsal bones and stretch them. The results of the reduction of fragments are monitored radiographically. Manual reposition often fails, especially with multiple fractures of the metatarsal bones. Reduction failures are associated with insufficient traction and difficulty in maintaining reposition of fragments in the repositioned position after termination of traction. As a result, when applying a plaster cast, secondary displacements often occur. If the reposition of fragments and keeping them in the correct position to produce using skeletal traction, these failures can be avoided. There are various ways of skeletal traction for fractures of the metatarsal bones. Most of them are based on stretching with silk thread or wire for soft tissues of the distal phalanges (Fig. 4.5). This method of extension, especially if it is carried out for a long time, carries the danger of the eruption of soft tissues, the formation of coarse scars at the site of extension and necrosis of the distal phalanges. The effectiveness of skeletal traction can be greatly improved by using the sliding tire Circassian-Zade (Fig. 4.6), which allows you to stretch directly over the bone of the distal phalanx using special taps. Patients in such a tire easily carry traction, move freely with crutches. The method of treatment after removal of skeletal traction is the same as for fractures without displacement. We give the observation. On the radiograph of the right foot (Fig. 4.7, a), a comminuted fracture of the IV and V metatarsal bones with displacement of fragments was found. Under local anesthesia (5 ml of a 2% solution of novocaine in the area of the fracture), the fragments were repositioned by pulling along the length of the injured fingers and pressure on the fragments in the direction opposite to the displacement. After that, 3 ml of a 2% solution of novocaine was injected into the region of the distal phalanges of IV and V fingers and skeletal traction was applied using special taps and a sliding tire of our design (Fig. 4.7, b). The tire is fixed to the foot with plaster bandages. The patient easily endured traction, on the 2nd day he was allowed to move around with crutches. After 3 weeks, the tire and the hoes removed. On the control radiograph, the displacement of the fragments of the IV and V metatarsal bones is eliminated, a mild callus is determined. Imposed plaster "boot" with built-in metal instep of our design. After removing it (after 6 weeks), physiotherapy exercises, massage, and swimming in the pool were prescribed. The patient began work after 2 months. Examined after 2 years (Fig. 4.7, c). No complaints, wears ordinary shoes, works on the same job. In case of multiple and open fractures and fractures of the metatarsal bones that are not amenable to reduction by conservative methods, treatment by distraction in the peripheral parts of the metatarsal bones or in the proximal phalanges has proven itself well. For the treatment of this method Yu.Yu.Kolontay et al. (1980) apply a special device. In the case of the ineffectiveness of the conservative method of matching fragments and the inability to apply the method of extra-focal compression-distraction transosseous osteosynthesis, one should resort to the operational adaptation of the fragments with their fixation using the metal rod of Bogdanov. Indications for intraosseous osteosynthesis: transverse and oblique fractures of the diaphysis of the metatarsal bones with displacement of fragments that are not amenable to closed reposition; fractures of the metatarsal bones in several places at the same time. Contraindications: intraarticular and longitudinal fractures of the metatarsal bones; fractures in the area of the necks and heads. The method of intraosseous fixation with a flat metal rod of Bogdanov consists in the following. Under intraosseous anesthesia with a 0.5% solution of novocaine on the dorsum of the foot, a longitudinal incision is made parallel to the damaged bone. Expose the fracture site; fragments are isolated and compared. Then, at the base of the broken bone, a hole is drilled with a thin drill or triangular awl, a metal rod is inserted into it, and it is passed through the fracture plane into the canal of the second fragment. Making sure that the fragments are correctly positioned, they bite off the outer part of the stem with nippers, and bend the end of it slightly, press it against the bone, and sew up the skin above it. After the operation, soft tissues are infiltrated with penicillin solution, a “boot” type plaster cast is applied, inserting a special metal instep in the plantar part. In patients with injuries of the metatarsal bones, there is usually no permanent disability even with incorrectly accrete or non-accrete fractures. The exceptions are fractures in which the displaced fragments form an angle open to the rear. Because of this, the patient cannot rest on the sole. The exact reposition of the metatarsal bone fragments is important for the preservation of the transverse and longitudinal arches of the foot, which play a crucial role in its function. Foot surgery |
| Read: |
|---|
New
- What you need for acrylic powder
- What does owl mascot mean
- Analyzes for pancreatitis: what research should be done and what indicators show
- Owl - a talisman to attract money and good luck
- What bird screams at night with a kitten's voice?
- Cholesterol and stress
- Manicure at home
- Effective facial
- What is a man after a broken leg?
- The trees and shrubs of the park survived the winter well