Site sections
Editor's Choice:
- How many grams of honey in a teaspoon and a tablespoon
- Pancreatitis tests: what studies should be done and what do the indicators say
- How to remove cholesterol from the body
- Hyperplasia of the cervix and endometrium: why treatment is necessary
- How much fracture is fused
- How do leaves change in autumn
- All you need to know about pumping honey
- Manifestations and recovery in case of marginal fracture of the first toe
- Wine fermentation at home
- Chicken with mushrooms - recipes with photos
Advertising
| Pancreas urine test. Pancreatitis tests: what studies should be done and what do the indicators say |
|
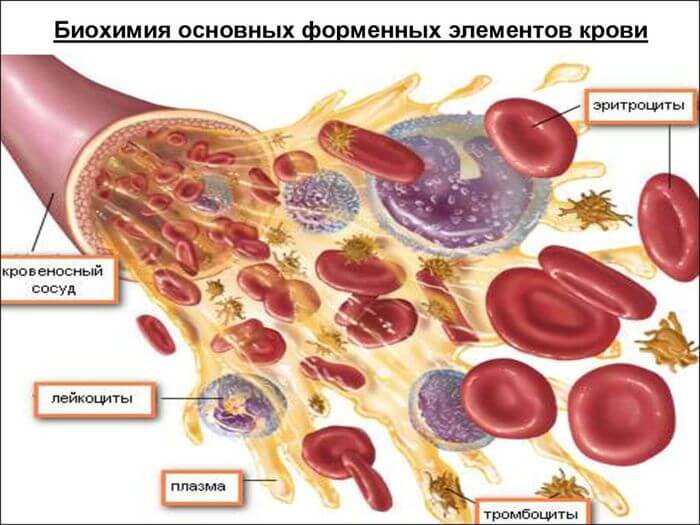
In the diagnosis of acute pancreatitis, the most popular test for more than 50 years is the determination of alpha-amylase activity in the blood and urine. In acute pancreatitis, the activity of alpha-amylase in blood and urine increases 10-30 times. Hyperamylasemia occurs at the onset of the disease (after 4-6 hours), reaches a maximum after 12-24 hours, then decreases rapidly and returns to normal on the 2nd-6th day. Hyperamilazuria usually lasts longer than an increase in serum enzyme activity. Serum alpha-amylase levels do not correlate with the severity of pancreatitis. More accurate information is obtained by studying the activity of amylase in the daily volume of urine. Alpha amylase activity is an important indicator, but not specific for acute pancreatitis. In addition to the pancreas, the salivary glands, lungs, and intestinal mucosa can be a source of amylase. Diseases that lead to an increase in blood amylase activity may include intestinal inversion, perforation of a peptic ulcer, cholecystitis and appendicitis. It was shown that only in 1/3 of patients with acute abdominal pain, an increase in amylase is due to pancreatic pathology. To increase the information content, it is recommended to combine the determination of blood and urine amylase activity with the determination of serum lipase activity, which is the most specific criterion, and with the parallel determination of creatinine concentration in urine and blood serum. Normally, the amylase-creatinine clearance indicator ranges from 1 to 4%. An increase of more than 6% suggests the presence of pancreatitis, since with pancreatitis, the level of true pancreatic alpha-amylase of saliva increases, and its clearance is 80% faster than the clearance of alpha-amylase. Recent studies have shown that the sensitivity of the diagnosis of pancreatitis in lipase is higher than in alpha-amylase. So, in patients with confirmed pancreatitis and with normal levels of alpha-amylase, lipase was increased in 68% of cases. It is very important to simultaneously determine both enzymes. The best diagnostic indicator for acute pancreatitis is a 5-10-fold increase in lipase activity, hyperamilasemia and an increase in amylase / creatinine clearance. Simultaneous determination of serum alpha-amylase and lipase allows with specificity up to 98% to diagnose pancreatic lesions. A specific diagnostic test in the laboratory diagnosis of acute pancreatitis is the determination of elastase activity in blood serum and feces. This indicator remains significant for several days even after a single attack of acute pancreatitis. Laboratory data can play an important role both in the recognition of acute pancreatitis and in establishing its shape, severity and prognosis of the disease. In chronic pancreatitis without exacerbation, the activity of serum pancreatic enzymes remains normal, and sometimes even reduced. With exacerbation of chronic pancreatitis, there is an increased intake of pancreatic enzymes in the blood, the so-called evasion of enzymes, which is caused by a violation of the integrity of the parenchyma of the gland and stagnation of secretion in a particular section of the pancreatic duct system. With severe pancreatic fibrosis, especially with fibrosclerotic chronic pancreatitis, the level of enzymes in the blood serum can be normal in most patients, even during an exacerbation. The activity of serum amylase begins to increase 2-12 hours after the exacerbation and reaches a maximum by the end of the day with a subsequent decrease in activity and normalization during the week. An increase in the activity of serum amylase by 2-3 times in combination with an increase in the level of lipase and trypsin is a reliable laboratory test of chronic pancreatitis. The pancreas is the only source of trypsin formation, and the determination of its activity can provide valuable information about the exocrine function of an organ. Along with the study of trypsin activity, the content of its inhibitor in the blood, as well as the inhibitor / trypsin ratio, are studied. A highly sensitive and specific test, indicating an exacerbation of chronic pancreatitis, is an increase in serum trypsin and a decrease in the concentration of trypsin inhibitor. This is especially true for interstitial-edematous forms of chronic pancreatitis, as well as for pancreatitis, combined with peptic ulcer of the duodenum or duodenitis. Of particular diagnostic value in the pathology of the pancreas is the determination of lipase activity in the blood. Clinical observations indicate an increase in blood lipase activity during exacerbation of chronic pancreatitis, especially with pancreatitis of cholangiogenic nature. During remission of chronic pancreatitis, amylase activity in the blood is within normal limits. With exacerbation of chronic pancreatitis, a number of patients experience hyperbilirubinemia, an increase in the serum activity of alkaline phosphatase and GGTF due to the development of partial or complete obstruction of the biliary tract associated with the presence of an obstruction in the area of \u200b\u200bthe large duodenal papilla (stenosis, stone, papillitis), reactive hepatitis or with compression distal section of the common bile duct of the inflamed and densified head pancreas. To study the exocrine function of the pancreas in clinical practice, a study of the activity of pancreatic enzymes in the blood and urine is carried out before and after the use of pancreatic secretion stimulants - the so-called test for evading enzymes in the blood after intravenous administration of secretin and cholecystokinin. The activity of pancreatic enzymes is normal after stimulation of the pancreas increases by no more than 2 times and after 2 hours it returns to its original level. In pathology of the pancreas, the activity of enzymes increases by more than 2 times and after 2 hours it does not return to the initial level. Additionally, you can use the proserin test. A study of the activity of amylase in the urine before and 2 hours after subcutaneous administration of 1 ml of a 0.05% solution of proserin. A positive test for the avoidance of enzymes in the blood and urine indicates involvement in the pathological process of the pancreas and serves as an indication for a more detailed examination of the patient. In feces, the activity of chymotrypsin and elastase is determined. These tests are used to reduce exocrine pancreatic function, as well as for the differential diagnosis of malabsorption syndrome. Determination of chymotrypsin activity in feces may be recommended as a search test. In chronic pancreatitis, 1 / 2-1 / 3 patients have carbohydrate metabolism disorders. In half of these patients, they show signs of diabetes. The basis for the development of these disorders is the defeat of all cells of the islet apparatus of the pancreas, resulting in a deficiency of not only insulin, but also glucagon. Insulin deficiency is detected by an increase in the amount of glucose in the blood. Pancreatitis tests - The most important stage in diagnosing the state of the pancreas. Making a diagnosis is a laborious process. Similar symptoms confuse the clinical picture. To reliably learn about the well-being of an organ, you need to pass urine, feces and blood, undergo an ultrasound, etc. The article highlights the key points of diagnosis: a list of analyzes with a breakdown of the results. woman working on a microscope Eine Anwenderin sitzt an dem Mikroskop The inflammatory process, progressing in, in many cases is accompanied by symptoms that can easily be attributed to congestion, fatigue, lack of sleep. Weakness, fatigue, weight loss, malfunctions of the digestive system - all this accompanies the everyday life of residents of the metropolis, who have a bite on the fly, drink coffee on an empty stomach, have little rest and leave a lot of time on the road. Diagnosis of pancreatitis includes blood tests , feces, urine. Insidiousness lies in the fact that the gland can endure addictions, neglect of meals, stress, but once “explode” and remind of itself with an acute attack. Suppressing severe pain, you will never return to your previous lifestyle. Since then, medicines will become your eternal companions. Any deviation from the diet will result in new attacks or worse - serious complications. What tests should be taken with pancreatitis Firstly? As a rule, when contacting a specialist, the patient receives a number of referrals to the research laboratory. Depending on the results obtained, the doctor is already deciding whether to do a deeper examination and proceeds from the individual aspects of each patient. The above analyzes are mandatory, and more complex studies (MRI, ultrasound, etc.) are scheduled later if necessary. Blood test for pancreatitis: indicators and their meaningA general clinical blood test allows you to suspect inflammation in the gland. However, to make a diagnosis solely from its results is incorrect. With pancreatitis, a blood test notes: Erythrocyte reduction; Hemoglobin decline; Increased ESR; The number of leukocytes that is overestimated many times; Increased hematocrit. Blood counts for pancreatitis change up or down. Normally, these criteria are: Red blood cells in men - from 3.9 * 10 12 to 5.5 * 10 12, in women - 3.9 * 10 12 to 4.7 * 10 12 cells / l. Hemoglobin in men is from 135 to 160, in women - from 120 to 140 g / l. ESR in men - from 0 to 15, in women - from 0 to 20 mm / h. White blood cells in men and women - from 4 to 9 * 10 9 liters. Hematocrit in men - from 0.44 to 0.48, in women - from 0.36 - 0.43 l / l. Clinical blood test for pancreatitis Is a supporting measure. For reliable diagnosis, it can be re-prescribed. Naturally, attention is also paid to other research methods, which will be discussed below.
The well-being of the whole organism turns out to be in full view when taking a biochemical blood test. In the inflammatory process, the following indicators deviate from the norm: Amylase of the pancreas - Pancreatic enzyme responsible for the breakdown of starch, increases. Other representatives of the enzyme group, such as trypsin, elastase, phospholipase, lipase, also increase. Insufficient synthesis of insulin causes an increase in glucose in the blood serum. Bilirubin changes to a greater side from the norm if the swollen gland blocks the bile ducts. In some cases, transaminases increase. Total protein decreases. Increased amylase - primary signwith pancreatitis in its chronic or acute manifestation. This enzyme helps break down carbohydrates. Lipase is responsible for the breakdown of fats. Trypsin and elastase are representatives of the group of proteases whose function is to break down the peptide bond of amino acids in proteins. Biochemistry for pancreatitis done within a day from the date of delivery of the patient to the hospital with an acute attack. During hospitalization, the dynamics of amylase is studied, preventing further attacks and complications. About this the doctor suggests her continued increase, coupled with severe pain. What tests are done for pancreatitis and cholecystitis still?The doctor may recommend taking other tests, for example, to determine the immunoreactive trypsin in the blood serum. Only in 4 out of 10 cases a positive result will indicate a pancreatic lesion. In others - that the violations affected other organs (renal failure, cholecystitis, hypercorticism, etc.). Trypsin Inhibitors Blood Level - Anotherblood test for pancreatitis , which shows the degree of gland dysfunction. The smaller the number of inhibitors, the less favorable the prognosis. Urinalysis for pancreatitis rarely prescribed because of its cost. Informative is not a common common, but one that determines the presence of trypsinogen in the urine. Trypsinogen is a proenzyme that is an inactive form of trypsin. Its content in the urine reliably confirms the inflammatory process. Failures in the digestive system will certainly affect the stool, so they resort to taking a test for feces. Attention is paid to criteria such as: Is fat present in feces; What is its color; Are there undigested fragments of food. All this indicates a malfunction in the digestive system, and a discolored stool means that the bile ducts are blocked. With inflammation, feces are poorly washed off the walls of the toilet. Due to excess fat it has a shiny surface. Its consistency is liquid, the urge to defecate is frequent. Defecation is accompanied by a pungent and unpleasant odor. Now you know,how to determine pancreatitis by analysis. However, it is better to leave this duty to your attending physician, who, having professionalism and medical knowledge, will not only make the correct diagnosis, but also draw up the correct treatment regimen. The key to effective and adequate treatment is the correct and accurate diagnosis. And the most effective method from the time of Avicenna to the present day can be called laboratory research methods. The indicators of urine, feces, blood tests will tell the doctor exactly where the patient has a problem, and what are the sizes of the lesion. A blood test for pancreatitis, the indicators of which are decisive, will indicate the presence of inflammation, its form and size of the lesion. Many diseases occur, without making themselves felt, pancreatitis is the trickiest of them. Symptoms of pancreatitis, especially of a chronic form, are more like signs of fatigue or overwork than a serious disease of the intracecretory organ. The anatomical features of the pancreas are such that even if the primary causes of pancreatitis are eliminated, those negative changes that already exist do not stop, but will continue to develop and grow. The insidiousness of the disease lies in its asymptomatic course, as well as in the mechanism of organ damage. The main cause of the inflammatory process in pancreatitis is one or another obstacle to the exit of pancreatic juice, saturated with enzymes. Unable to pass through the pancreatic ducts, they begin to corrode the tissue of the gland itself, that is, autolysis occurs. But even this is not so much dangerous to humans, as the fact that all products of the inflammatory process with blood flow and the lymphatic system spread throughout the body, which can cause general intoxication.
If the patient complains of weakness, fatigue, weight loss and diarrhea, even if palpation does not confirm any specific syndrome indicating pancreatitis, he is first prescribed a biochemical blood test, blood for clinical trials, and feces and urine tests. Why do I need a general blood test
As already mentioned, the products of inflammation quickly spread through the circulatory system. Even if the patient does not yet experience any discomfort, the doctor will find signals in the clinical blood test that there is an inflammatory process and its intensity. It will also find out whether dehydration is present in the patient, which is relevant against the background of intestinal upset. The development of pancreatitis is also evidenced by such indicators as:
Blood for clinical analysis is taken from the finger, on an empty stomach. Results can be obtained within a few minutes if the laboratory has a special apparatus, or during the day if the analysis is performed manually by the laboratory assistant. No preliminary preparation is required from the patient, other than observing a 6-hour abstinence from food and drink. Control analyzes of clinical indicators of blood are always done at the same time, since their level in pancreatitis can vary throughout the day. The value of biochemical analysis of blood
What biochemical blood tests for pancreatitis can show will immediately tell the specialist about the extent of damage to the pancreatic cells, disorders of intracretory and exocrine activity, the presence of an obstruction in the biliary tract. If pancreatitis is suspected, the doctor draws attention to such analysis results as:  A detailed biochemical blood test is able to give a complete picture and show the form of pancreatitis. The indicators show the presence of an acute attack of pancreatitis or a prolonged course of a chronic form with pancreatitis. Other studiesDespite the crucial importance that a biochemical blood test for pancreatitis has, other tests are prescribed to confirm the diagnosis, for example:
Urinalysis for quantitative trypsin is a highly specific and most accurate indicator. But, unfortunately, it is not available to all clinics because of expensive equipment and the high cost of analysis. Since the main task of the pancreas is to ensure the normal digestion of food, the analysis of feces is of great importance. According to its results, the functional ability of the organ, the size of the lesion in pancreatitis, the degree of digestion and assimilation of the food received are determined. The pancreas performs one of the important functions in the system of the gastrointestinal tract, and produces pancreatic juice. This substance contains digestive enzymes, which provide the breakdown of proteins of fats and carbohydrates for further absorption by the body. Pancreatitis is an inflammation of the pancreas. Over the past 40 years, cases of this disease have doubled. How to determine pancreatitis in the laboratory? DiagnosticsThe patient is referred to a doctor with suspected pancreatitis specific symptoms. If the disease proceeds in an acute form, the signs of pancreatitis are bright, the pain syndrome is severe. In a chronic disease, the symptoms are not so prominent, but malaise is constantly present. The following symptoms indicate pancreatitis:
After a visit to the doctor, a medical history is collected, the patient's complaints about the state of health. Based on the results of the examination, appropriate laboratory tests are prescribed. If pancreatitis is suspected, general and biochemical blood tests are mandatory. Urine analysis, fecal analysis, radiography, saliva analysis and others can also be prescribed. General analysisIn a general blood test, there are a number of indicators that can indicate the development of a disease in the patient's body. Despite the generalized data, the level of leukocytes, erythrocytes and ESR is noted in the blood test. A biological sample, as a rule, is immediately submitted for general and biochemical analyzes.
What indicators are used to diagnose pancreatitis in a general blood test:
A clinical blood test for pancreatitis and indicators are generalized and do not allow to establish a diagnosis. A general study is auxiliary, confirming the results of biochemistry. At the same time, the studied parameters make it possible to find out the general state of the patient’s health and evaluate the effect of the disease on the body. BiochemistryBiochemical research is a complex process that can contain a huge number of indicators of the studied parameters. For the diagnosis of pancreatitis, only some of them are used. A blood test for an acute disease is performed within a day from the moment the patient contacts the medical facility. It is necessary to determine the following indicators:
Analysis of urineA urinalysis is quite informative for the doctor. A biological sample is collected by patients at home on their own and delivered to the laboratory for analysis. Previously, the doctor will give instructions that should be followed to obtain the most reliable information on the results of the study. The following parameters of the biological sample are taken into account:
Fecal analysisChanging the structure of cola is one of the symptoms of pancreatitis. It is this type of study in an actual form that reflects the functional level of the pancreas. If the secretion of digestive enzymes produced by the gland is reduced, then pancreatitis can be diagnosed.
With pancreatitis, the following manifestations are observed:
As additional research methods, various types of tests for pancreatitis can be used. For example, analysis of saliva helps to detect the concentration of pancreatic enzymes. According to the result of this analysis, one can find out the severity and degree of development of pancreatitis. Also, this type of study greatly simplifies laboratory diagnostics and allows you to monitor the dynamics of pancreatitis. Pancreatitis is a serious pathological condition that can lead to serious consequences for the body. If specific symptoms of pancreatitis are detected, you should immediately consult a doctor for help. Conducting laboratory tests will not take much time, but will help to establish a diagnosis in a timely manner and choose the most effective treatment. Pancreatic inflammation, which causes severe disorders in the body, is most often manifested by pancreatitis. Pancreatitis is acute, and with the recurrence of attacks 2-3 times a year, it becomes chronic. It is caused by various reasons. For successful treatment, the causes of the disease must be eliminated. To eliminate them, the patient needs to be thoroughly examined. Pancreatitis tests are an important part among all methods of examining a patient. Deviation from the norm in terms of blood, urine, feces indicates the development of the inflammatory process in the pancreas. What tests are done with pancreatitis, the doctor determines. Often these are:
Clinical analysisMetabolism in the body lays its mold on the blood. Therefore, her study is an important diagnosis of the patient's condition. As part of the overall review, elements familiar to everyone:
In addition to them, the research indicators contain:
All indicators have a norm, deviations from it in the blood test make it possible to suspect the inflammatory process in the body, which requires additional studies. Blood biochemistryAccording to the results of the testimony in the blood test, if the doctor correctly decrypts them, one can judge the health of each organ and all systems of the human body. Deviations from the norm inherent in healthy people help determine the active inflammatory process and establish the stage of the disease.
Biochemical research has many positions, and a specific doctor can include only those positions that are important, in his opinion, in the diagnosis of the disease. It includes indicators:
Behind each position is a specific organ that produces trace elements in the blood. Deviation from the norm makes it possible to assume inflammation of such. A biochemical blood test for pancreatitis uses the following positions:
FecesThe study of feces for the recognition of malfunctions in the pancreas is of minimal importance. Decreased secretion affects fat processing. In feces observed:
UrinalysisThe level of diastase, it is also amylase, in the urine is evidence of pancreatic disease. Exceeding the norm by 250 times is noted. Its increase is associated not only with pancreatitis, but many other factors. Therefore, with an increased level of diastasis, data from other studies are needed. The decrease in diastase volume is explained by failures in enzyme-forming activity. From the entire list of positions, we select only those that can indicate pancreatitis:
The ambiguity in the interpretation of a particular research position dictates the need for additional tests to clarify the result. Important Diagnostic TestsTo show an accurate diagnosis of pancreatitis, research methods are supplemented by various laboratory tests. Popular tests from various options:
A glucose tolerance test will determine the disorder in the synthesis of insulin by the pancreas. Perhaps many did not suspect that such tests and tests could be taken. Caring for his health, the patient himself can ask the doctor about the appointment of such studies. Laboratory studies complement the diagnosis of pancreatitis, being an important part of the overall comprehensive examination. There are many positions in laboratory studies, however, indicators of enzyme volumes in the blood are of maximum importance to the doctor. In the course of 1 day - pancreatic amylase, after a few days control - elastase and lipase. In chronic pancreatitis, their value of the norm and deviations is different than in acute course or remission. To show which disease is haunting you, whether it is pancreatitis, what stage: exacerbations or remissions, what are the predictions for its cure - all questions have an answer in clinical tests, additional tests and tests. |
| Read: |
|---|
Popular:
How hair straighteners work
|
New
- Food Sources of Ascorbic Acid
- The most dangerous poison for humans
- We study a tree, playing: riddles about a birch
- Plaster cast care
- How to moisturize dry skin in the winter
- Fish oil Biafishenol: instructions for use
- How to clean the apartment yourself from damage
- Amanita mushroom - healing properties, how to take tinctures and prepare ointment
- Pelvic injuries
- Nail extension devices: a list of everything you need
 Biochemical blood test for pancreatitis
Biochemical blood test for pancreatitis
 The results of a biochemical blood test are the main and decisive facts in the diagnosis. This study allows you to accurately determine the degree of work of each organ in the body and the size of the disorders caused by inflammation.
The results of a biochemical blood test are the main and decisive facts in the diagnosis. This study allows you to accurately determine the degree of work of each organ in the body and the size of the disorders caused by inflammation.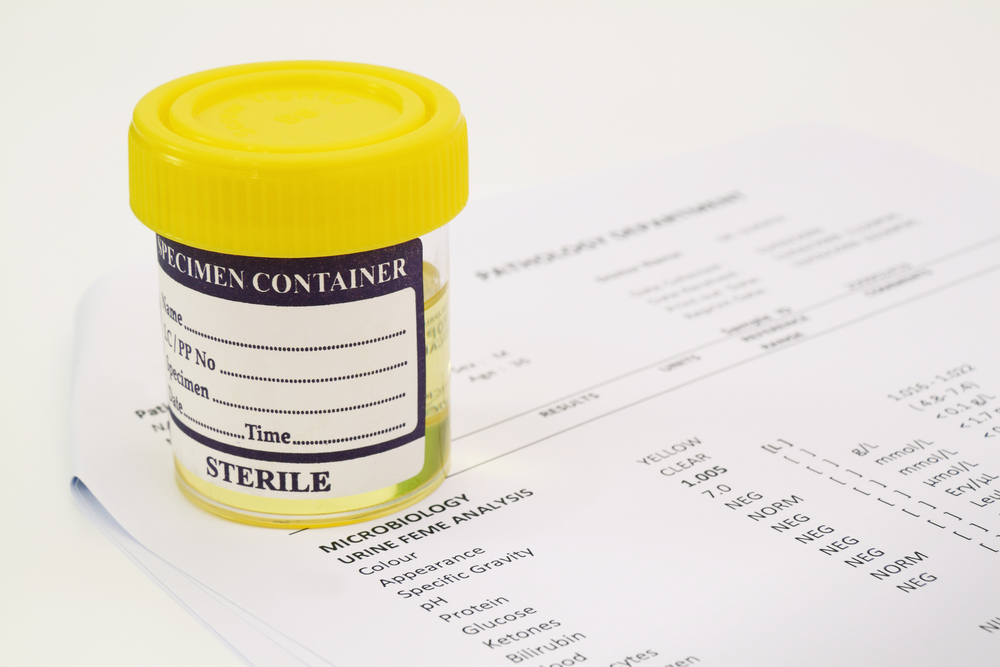 Of no less importance are analyzes of other biological media. So, urine and feces in pancreatitis can give 100% guaranteed confirmation.
Of no less importance are analyzes of other biological media. So, urine and feces in pancreatitis can give 100% guaranteed confirmation.