Site sections
Editor's Choice:
- How much fracture is fused
- How do leaves change in autumn
- All you need to know about pumping honey
- Manifestations and recovery in case of marginal fracture of the first toe
- Wine fermentation at home
- Chicken with mushrooms - recipes with photos
- Treatment and rehabilitation for knee fracture
- Chicken fillet with porcini mushrooms in a pan
- What drugs lower cholesterol
- How to accelerate the healing of a leg fracture
Advertising
| Stages of bone fusion after fracture. How much fracture is fused |
|
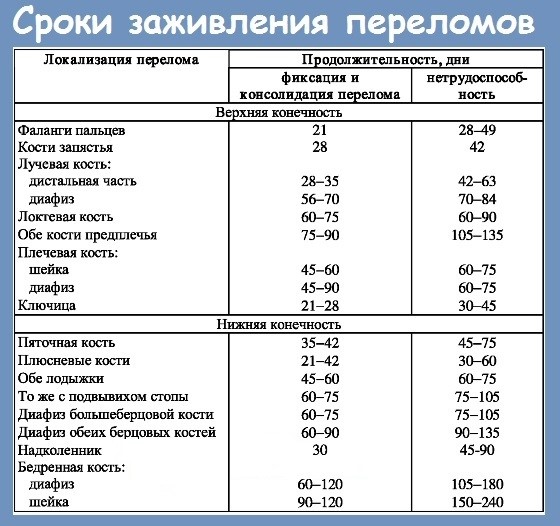
Throughout life, everyone can experience a fracture of any part of the body. Such an incident in many people always raises questions - how do bones grow together, how long do bones grow together, how severe are the consequences of a fracture. Such injuries occur in different situations, while for some time they deprive a person of disability, which is a multiple inconvenience. This is such a widespread damage that every person should know how a person heals bones after a fracture, how much gypsum should be worn, and how to speed up the healing period. The fracture classification table includes the most diverse types and stages of these lesions. How many fractures grow together, not a single orthopedic surgeon or traumatologist can tell, because these are individual indicators that depend on many different factors. In adults, the fusion of bone fractures takes a much longer period than in children, due to an insufficient amount of calcium in the body. If the child broke his arm, or other limb, his bones not only grow together much faster, but also most likely without complications. The child’s body is much faster regenerated and restored than any adult. How long does the fracture splicing lastA broken bone is restored in each person individually with a different time interval. There are various factors that accelerate or slow down the process of fusion. For example, small bones heal much faster than large ones. How long the fracture heals depends on the person’s age, immunity, and lifestyle. Also, how much longer the bone will heal after a fracture depends on the location of the damage itself.
Often people wonder how long a leg fracture heals. In order for bone fusion after a fracture to occur faster, it must be in full fixation and immobility. Such conditions cannot be created for all parts of the body. Although a broken leg is fixed with plaster, it is still subject to some pressure than other limbs. Therefore, the healing time for fractures on the leg requires 3 or more months, the hand is restored in just 2 months, and the healing of a broken phalanx of the fingers requires only a couple of weeks. In children, these processes occur much faster. If this is a fracture of the femoral neck in elderly patients, then this damage has not only long periods of fusion (up to 1 year), but can also be fatal for the victim (in 10-20% of cases). This type of fracture often requires surgical intervention by qualified specialists. In children, the femur heals together more quickly over several months. If the fracture is accompanied by ruptures of tissues and muscles, as well as the presence of displacements of broken bones and a large number of fragments, then the recovery time increases. It is important during recovery to exert a minimum of pressure on the hips and not expose them to stress. Each patient wants to know how long the fracture heals. A long recovery period for any age is required for a fracture of the spine. It is impossible to say how quickly the bones heal in this case, since the area of the spine that has been injured plays a big role. Of great importance on how long the bone fusion after a fracture lasts is the presence of chronic diseases or diseases in the acute period of development. At this time, there is a violation of the immune system in the human body, which not only slows down healing, but also increases the risk of complications and consequences after an injury. Particular attention is required not only to the recovery period, but also how the fracture heals. Regardless of the severity, broken bones must be fixed in a fixed position using a plaster cast. Fixation is necessary solely for the purpose of proper fusion of tissues, bone and its fragments. You need to wear a plaster cast for the entire healing period of the injured area. First aid for a fractureAn important role in the speed of fusion of broken bones is affected by first aid for fractures. If this is an open fracture, it is very important that the infection does not get into the wound, in order to avoid inflammation and suppuration in this area. Therefore, the damaged area must be decontaminated, for this the circumference of the wound should be treated with an antiseptic, and covered with a sterile cloth until the team of doctors arrives.
A broken bone must be immobilized, for this, fixation is carried out using a medical tire or a simple improvised item - a board, plywood, etc. fixed on the injured area with a bandage. Only after this, the victim can be transported to the hospital for examination by a doctor and further treatment. If a person has a spinal injury, then solid stretchers or improvised means, for example flat boards, on which the patient must be carefully laid, are used for transportation. The timing of the consolidation of fractures directly depends on the provision of first aid and the emergency transportation of the victim to the hospital. Healing mechanismFusion splicing begins immediately after injury. Splicing can be of two types:
The mechanism of fracture fusion is very complex, therefore it is divided into certain stages:
At the end of all stages, the fused bone regains its strength, and is able to withstand various loads. ComplicationsThe risk of complications depends primarily on the correct first aid, and the qualifications of the doctor conducting the course of treatment. Complex injuries include:
The treatment of such injuries not only requires more time, but can also take place with certain complications:
Now, almost every person can observe a lack of calcium, phosphorus and other important trace elements in the body. The reason for their lack is the use of low-quality food. This significantly increases the frequency of fractures in the adult population and is directly related to the development of osteoporosis (loss of bone strength). In children, the body is in the process of growth and has a much larger number of useful elements, so their recovery takes less time. How to speed up bone fusion
Although the process of bone fusion during a fracture is lengthy, there are still ways to speed it up. To do this, you should adhere to some recommendations:
Careful implementation of all these points will certainly speed up the recovery process, and the bone will grow together quickly and correctly. Folk remedies
Over the years, people have also gathered tips on healing bone tissue. Some of them will be useful to familiarize yourself with:
Fusion of broken bones is a rather long and complex process, which is greatly influenced by multiple factors. By listening to the recommendations and following the requirements of doctors, you can help the bones to heal faster. ≫ More information Most broken bones heal completely without Deformation - especially in children. But in adults with poor health and poor blood circulation, bones often fail to grow together correctly. A broken bone begins to heal immediately after a fracture. Fusion fracture goes through four main stages. Stage One: Clot FormationFirst, blood collects at the ends of a broken bone, forming a viscous mass called a clot. From the clot, fibers are formed, which become the basis for the growth of new bone tissue. Stage two: healing cells fill the clotSoon, the cells that heal the bone - osteoclasts and osteoblasts - fill the clot. Osteoclasts begin to smooth the jagged edges of the bone, and osteoblasts fill the gap between its ends. After a few days, a granular bridge connecting the ends of the bone forms from these cells. Stage Three: Bone Callus Formation6-10 days after the fracture, the granular bridge from the cells becomes bone mass, called corn. It is fragile and with a sudden movement can break. This is why a broken bone must be motionless during healing. Later, the corn turns into hard bone. Stage Four: Fusion of the Ends of the Bone3-10 weeks after the fracture, new blood vessels begin to deliver calcium to the fracture site. It strengthens new bone tissue. This process, called ossification, connects the ends of the bone. After this, the bone becomes strong and is considered healed. Although gypsum can be removed, it will take about a year for the healing bone to be as strong as before the fracture. J. Zekkardi “How the fracture heals” - article from the section Emergencies in Surgery How long does it take to heal the bones after a fracture?A fracture is a serious injury, after which a full recovery occurs only when the bones are fused. But it can last quite a while. And what is the time of bone fusion during a fracture? What influences him? How to speed up this process? What happens with intergrowth?This process is quite complicated. So that you understand how the bones heal during a fracture, we suggest that you familiarize yourself with the stages of their fusion:
Splicing timeEven an experienced specialist cannot name the exact dates, since it depends on many features. But the approximate time of splicing can be called. For example, the scaphoid will grow together for about a month, the collarbone can grow in 3 weeks, the tibia will heal for about two months, and the femur as much as 2.5-3. What does splicing time depend on?Someone has a full recovery in a month, while others go in a cast for two months. And what does it depend on? We list the main factors:
How to speed up splicing?
ethnoscienceOur grandmothers also used some recipes for healing bone tissue. We offer some tools to you:
Summing up, we can say that bone fusion is a complex process that is influenced by many factors. But the tips will help you recover. To make the bones heal quickly - Home Treatment at KRASGMU.NETThe main objective of the treatment of bone fractures is the complete fusion of bone fragments and the restoration of lost function. In order for the bones to grow together quickly and correctly, it is necessary to follow the various recommendations presented in the article. Sometimes the bones do not grow together for a very long time, and you have to go in gypsum for months, especially for older people. For bones and joints to recover faster, they need minerals and vitamins. Fracture is a complete or partial violation of the integrity of the bone resulting from an injury. Fractures are open and closed. With an open fracture, a violation of the integrity of the skin is observed. A wound surface forms and infection can occur. Naturally, this leads to various complications and a slowdown in recovery. With injuries, bone cracks and tearing of bone tubercles can also form, to which muscles are attached. Perhaps a combination of a fracture with a dislocation. With age, bones in humans become lighter and thinner. So, in a seventy-year-old person, the skeleton is about a third lighter than in a forty-year-old. This decrease in bone density, or osteoporosis, occurs when the balance between natural destruction and bone repair is disturbed. Almost all older people suffer from osteoporosis, but in a different form: the disease is more severe in people who are thin and inactive, especially if their relatives are also affected by osteoporosis. Many do not suspect that they are sick with osteoporosis until, during a normal fall, they break their wrist or femur. Such a fracture can bed an elderly person and even prove to be deadly for him. The younger and stronger the body, the faster the bone fusion in fractures. Therefore, in children and young people everything comes back to normal much faster than in the elderly. There are no standards for bone fusion after fractures. In some, the bones grow together in a few weeks (3-4 weeks), in someone in 2 months, and in someone with the same fracture, the bones will heal for 1.5 years. In case of fractures, without bone displacement, as a rule, outpatient conservative treatment is prescribed. The principles for treating fractures are simple, with the restoration of bone integrity being most important. A fixative dressing is usually applied to the patient, usually a plaster cast. This allows you to reduce pain and ensure limb immobility. For fractures with complications, for severe fractures with bone fragments, with displacement, surgery is performed. In the most severe cases, fixation with metal knitting needles is used. Is it possible to accelerate the fusion of bones in fractures?Is there any way to speed up the process of bone growth? Yes, it can be influenced. Below are some helpful suggestions:
Physiotherapy for bone fracturesTo more quickly go through the process of bone fusion, physiotherapy is prescribed. Physiotherapy should be started already on the 2nd – 5th day after the injury. For pain relief, elimination of edema, resorption of hemorrhages and acceleration of bone regeneration, the following are used: UHF therapy, which has an analgesic effect, reduces tissue swelling, low-frequency magnetotherapy, interference currents. For a long time, bone tissue was looked upon as a very passive substance, unable to produce electrical potentials. And only in the middle of our century, researchers found that in the bones, as well as in other organs, electrical processes occur. A change in the nature of electrical signals was also observed with the introduction of metal screws into the bone, which usually fix the metal structures used to treat fractures. Interestingly, the ability to generate biopotentials under the load was also preserved in bones extracted from the body, and even in specially treated bones, in which only the “bare” crystalline base, the so-called matrix, remained. Analyzing these data, experts came to the conclusion that there are structures in the bone tissue that work as peculiar piezocrystals. Weak currents can have a noticeable effect on the regeneration of bone tissue, the available information allows specialists to apply electrical stimulation in the clinic for targeted exposure to bone tissue. Doctors know that the absence of a load on a damaged limb, its prolonged inaction slows down the formation of a full bone adhesion after a fracture. Therefore, it is recommended to move the damaged limb, naturally, within reasonable, permissible limits. But there are times when even minimal movement is impossible. If, in such a situation, the injured limb is affected by an electric current whose oscillation frequency coincides with the oscillation frequency of the biocurrents that occur in the bone during exercise, there is a positive dynamics. At the same time, immobility is maintained and the bones get the load they need. And as a result, the process of formation of bone adhesions is faster. Even in the Soviet period, Russian scientists developed techniques that allow the use of electro-current of directional action in case of fresh fractures, when for some reason the adhesion of bone fragments is disturbed, as well as in non-adherent fractures, false joints, and some bone defects. Clinical observations have shown that in many cases, which doctors call difficult, electrical stimulation gives a good result. What to do to make the bones grow together fasterCurrently, there is a tendency to lengthen the terms of adhesions of fractures. This is associated primarily with the widespread inadequate intake of such elements as calcium, phosphorus, etc. And also, the spread among the population, especially in people over 50 years old, of vitamin D deficiency, which ensures the flow of calcium from the intestine into the blood and then into the bone . In addition, vitamin D enhances the formation of a number of substances that are necessary for the normal fusion of a fracture. Calcium carbonate-based preparations (purified chalk) + Colecalciferol (vitamin D3) will help accelerate the healing of damaged bones. At the same time, there is an acceleration of fracture adhesions by 30%. Calcium is also involved in the regulation of nerve conduction, muscle contraction and is a component of the blood coagulation system. Vitamin D3, regulates the exchange of calcium and phosphorus in the body (bones, teeth, nails, hair, muscles). Reduces resorption (resorption) and increases bone density, filling up the lack of calcium in the body, is necessary for the mineralization of teeth. Vitamin D3 increases the absorbability of calcium in the intestine. The use of calcium and vitamin D3 prevents the production of parathyroid hormone (PTH), which is a stimulator of increased bone resorption (leaching of calcium from the bones). During the recovery period after a fracture a complete set of vitamins and trace elements is needed. Nutrition for fracturesIn order for the bones to grow together faster, there should be enough calcium, vitamin D and protein in the diet. Every day, it is advisable to drink a glass of any fermented milk drink - kefir, yogurt, and eat 100 grams of low-fat soft cottage cheese. In order for calcium to be better absorbed, vitamin D must also be present in food. It is abundant in cod liver oil and fatty fish. For fractures, the body needs protein, because it is one of the building materials of bone. The protein is rich in solid low-fat cheese, low-fat poultry, meat, fish, eggs. Poultry and meat is healthier to eat boiled. For fractures, you need to eat foods with gelatin (meat aspic). For bone fractures do not limit sweet. The human body cannot do without a sweet. Sugar contains sucrose, which contributes to the rapid accretion of bones after fractures. Physical activity in fracturesPhysical activity is necessary for the bones to grow together faster. However, thinned bones require a number of limitations in the exercise program. You will need the advice of a physical culture specialist and a physiotherapist. You can try to exercise in a group. You can walk half an hour 3-5 times a week. During the post-fracture recovery period, it is important to speed recovery and alleviate the pain associated with the fracture. Exercise will not only speed up the recovery process, but also help reduce the risk of subsequent damage (fracture) in the event of a fall, as well as improve balance, posture, flexibility and coordination of movements. Make walking a must part of your daily life. Bad weather or slippery streets should not be an obstacle: you can walk at home, in large stores or other indoor areas. If exercise is difficult for you, you can do it every other day. Always listen to your body. Physical activity improves the physical condition: physically active people have more energy and they do not get tired as quickly as less active people. In other words, physical activity helps to feel better and get more out of life. Summarizing, we can say that the accretion of bones is a complex process that is influenced by many factors. But our tips will help your bones grow together faster. how many bones coalesce after a jaw fractureRider ... The bone accretion after a fracture is accompanied by the formation of a new tissue, as a result of which a callus appears. Each fracture is unique, as each human body is unique, therefore the timing for restoring bone integrity can vary within very wide limits. Some bones can grow together for more than six months, others - only a few weeks. The recovery rate is directly influenced by the patient’s age and the severity of the fracture. Instruction
Callus formation is not necessary to heal a fracture. Providing perfect comparison of fragments, tight contact between fracture surfaces and ensuring their complete immobility, preserving or quickly restoring a sufficient level of blood supply (in some types of osteosynthesis), there is direct restoration of the continuity of osteons of the compact substance of bone fragments - primary fusion. This fusion without prior formation of periosteal corns and without the participation of cartilage and fibrous tissue or coarse fibrous bone. Radiographically, it manifests itself in the disappearance of the fracture line within a few weeks without the formation of visible callus or with the formation of a barely noticeable callus. Callus is formed if the listed conditions of primary fusion are absent. The processes occurring in the first stage in the x-ray image remain invisible. Sometimes it is possible to observe the expansion of the fracture line in the first days, due to bone resorption at the ends of the fragments. This is practically important in those rare cases when the fracture line is not detected in the first image, but becomes visible after 10-12 days due to such resorption. The proliferating cells of the periosteum, endosteum, and bone marrow are differentiated, provided there is sufficient blood supply to the osteoblasts that set aside bone tissue. Reticulofibrotic osteogenic regenerate is converted to bone regenerate. Since angiogenesis in the damage zone occurs more slowly than cell proliferation and differentiation, they are converted rather into chondroblasts and chondrocytes. Thus, the regenerate consists of three components: reticofibrous osteogenic, cartilage and fibrous tissue. Under unfavorable conditions of regeneration (slow restoration of blood circulation, mobility of fragments), the ends of fragments are connected and immobilized mainly by cartilaginous periosteal corn, which, unlike bone spur, does not need intensive blood supply. As angiogenesis increases, cartilage tissue is converted into bone by enchondral ossification. Radiological signs of reparative bone tissue regeneration appear in the second stage. The first sign of fractures of a diaphysis of long tubular bones the appearance of bone bridges or bridges between the ends of fragments overlapping the fracture line along the periosteal surface of the bone ( periosteal callus). It is most pronounced in fractures of the diaphysis, where the periosteum is more active. The same bridge, but usually less pronounced, can be detected on the endocortical surface ( endoscle callus). Endotal callus from the very beginning is bone. Thus, the callus is a kind of “patch” on the bone connecting the fragments. Callus initially consists of a coarse-grained, primitive, usually weakly mineralized bone ( primary callus), which subsequently undergoes resorption and is replaced by mature lamellar bone tissue ( secondary callus). It should not be confused with the primary and secondary fusion of fractures. Primary corn on radiographs looks friable, tender. Detection of periosteal and endosteal corns on radiographs does not mean fusion of fragments. The role of the callus is that it fixes the fragments, connecting their ends and thereby providing the immobility necessary to restore bone continuity ( secondary fusion). In conditions of the continuing mobility of fragments, the regenerate is subjected to injury, and the process of bone tissue regeneration is disturbed. Thus, the presence of a pronounced periosteal callus indicates an inadequate reposition or insufficient stability of the bone fragments that have occurred from the very beginning, or the secondary displacement of the latter that has occurred. In oblique and spiral fractures, an endosteal callus predominates, while a periosteal one is small. If the gap between the fragments passes obliquely with respect to both the frontal and sagittal planes, thin periosteal bridges often do not reach the contour on radiographs in standard projections. Conversely, the projection imposition of the sharp end of the fragment on the end of the other fragment, especially if there is a slight lateral displacement, can simulate a bone bridge. In such cases, additional radiographs in oblique projections are needed to bring the bone bridge, which overlaps the fracture line, into a marginal position. Such radiographs are particularly useful in the case of projection overlay metal structures. If the appearance of callus on radiographs is delayed with respect to clinically determined fixation of fragments, this reflects a delay in the conversion of cartilage to callus callus and indicates less favorable conditions for the healing of the fracture (primarily to maintain some mobility of fragments). Mineralization of the callus itself occurs quickly, including in patients with osteoporosis. The exceptions are patients with impaired phosphorus-calcium metabolism, and above all with a deficiency or impaired metabolism of vitamin D. The volume of periosteal corns is mainly proportional to the degree of fragment displacement. With a significant displacement, the corn is formed in para-soft soft tissues. In this case, the periosteal and parostal corn, developing along the lateral surfaces of the bones, provide not only fixation, but also fusion of fragments. A massive callus with a continuation of the gap between fragments with a small displacement may serve as an indication of the instability of the fracture area. In the presence of angular displacement of fragments, such a corn is more developed from the side in which the angle is open. Fixation of fragments creates conditions for development intermediary cornformed directly between the fracture surfaces (the third stage of fusion). Intermedia callus is always primary bone and is formed by desmal type. For the formation of an intermediary corn, a gap between fragments of at least 100 microns wide is necessary. With a smaller gap, germination of the regenerate into it is difficult and time is required for its expansion (resorption of the ends of fragments). Fusion fracture, meaning the restoration of the continuity of bone tissue between the fracture surfaces, is precisely due to the intermediary corn. Periosteal and endosteal callus are temporary formations that undergo a more or less pronounced reduction after the formation of a solid intermediary callus. In X-ray imaging, the formation of an intermediary corn is manifested by a gradual deterioration in the distinctiveness of the fracture line, a loss of clarity of facing each other surfaces of the ends of fragments. From the point of view of the clinician-traumatologist, fracture adhesion implies a sufficiently strong connection between the fragments, which allows subjecting the extremity to mechanical stress. Such conditions are created when a strong periosteal and endosteal callus has already formed. A moderate mechanical load cannot damage the intermediary corn. In assessing the healing of a fracture, traumatologists are guided by the time limits established by experiment with each localization of the fracture. However, radiography provides important information. Both clinical signs and radiological ones are taken into account: the severity of periosteal corns, its density and extent along the bone circumference, the width of the gap between the fragments. The replacement of a poorly mineralized primary corn with a secondary corn from lamellar bone can be to some extent judged by the increase in the density of corn. As radiographic signs of sufficiently strong fixation of fragments, periosteal callus density approaching cortical bone density can be considered, and the width of the gap between fragments is no more than 2–3 mm. Under these conditions, it is possible to proceed to a cautious and gradually increasing load of the limb, including the static load of the lower limb in a plaster cast. Despite the formation of a solid intermediary corn and the restoration of bone continuity, the fracture line can still be traced for a long time. This is due to the fact of an earlier replacement of the coarse-fibrous bone by the lamellar bone in the periosteal and endosteal callus than in the later forming intermediary callus. While this replacement process continues, the weaker mineralization of the coarse-fibrous bone as compared with the lamellar one, as well as the gradual resorption of the former, cause a lower density at the site of the fracture line. With the onset of mechanical stress occurs restructuring of the resulting callus - resorption of excess bone tissue, adaptation of the trabecular structure to the load conditions with thinning and complete resorption of some trabeculae and thickening of others. This process (the fourth stage of fusion) lasts for months and years. With bone fractures with spongy structurewhere the main mechanical value is not the cortical layer, but the network of bone trabeculae and the low-active periosteum, the periosteal callus is weakly expressed and often in the X-ray image is often not captured. Since this causes fractures of a large number of bone trabeculae, restoration of the continuity of the trabecular network occurs due to multiple endosteal calluses. The source of bone tissue regeneration, the bone beams, is endost. Fusion of such fractures occurs on the desmal type, without an intermediate cartilaginous stage, as in microfractures. In assessing the healing of such fractures, it is not necessary to focus on the visible signs of adhesion. It is more correct to ask the opposite question: are there any signs indicating that the fracture is healing? not happening? These signs include: increasing demarcation of the ends of fragments with their underlined edges, compaction at the edges of fragments and expansion of the fracture line. The absence of signs of non-union fractures in these parts of the skeleton may be the only evidence that the fracture is consolidating. In addition, in the process of healing such fractures, a transverse band of a cancellous bone seal may appear, which was absent in earlier photographs (endosteal callus). At the same time, the previously determined fracture line and other density changes disappear: with impression fractures, a compaction zone that reflects the zone of compression of the bone beams; Note the most significant factors that worsen the conditions of healing.
Healing occurs the faster, the larger the surface area of the fragments, the weaker the muscles, the contractions of which can interfere with the stability between the fragments and cause them to shift, the smaller the lever that can increase the force of the muscles. The rapid healing of fractures in the spongy part of the articular ends of the bone is favored by the large surface area of the cancellous bone. For example, healing of a fracture of a radial bone in a typical place occurs quickly, because The surface area of the ends of the fragments consisting of the spongy bone is large, and the lever, which increases the force of the muscles, is short. With "long" oblique fractures of the femur diaphysis, fusion conditions are more favorable than with "short" oblique or transverse fractures due to a larger surface area of the ends of the fragments and a shorter lever. In case of intertransverse fracture of the femur, the surface of the ends of the fragments is large, but due to the strong muscles of the thigh and a large lever (these muscles are attached far from the fracture site) there is a threat of displacement. |
| Read: |
|---|
Popular:
Handbook for kissing a woman's hand
|
New
- How to moisturize dry skin in winter
- Biafishenol fish oil: instructions for use
- How to independently clean the apartment from damage
- Amanita mushroom - medicinal properties, how to take tinctures and prepare ointment
- Injured with pelvic injuries
- Devices for nail extension: a list of all necessary
- Owl tattoo and its meaning for girls and guys
- Chicken with honey and mustard
- Is a single kidney pregnancy possible?
- Varnish for stone with a wet effect