Site sections
Editor's Choice:
- How will your prayers and conspiracies attract good luck in love?
- Family peace conspiracy for a picture
- Gothic tarot vargo Gothic tarot joseph vargo interpretation of cards
- The principles of making money in the family according to the Vedas Too big requests
- Rolling out cancer, damage, evil eye and other serious diseases
- Diagnostics and cleaning of negative bindings: rolling out spoilage with an egg
- What can spoilage on bread do
- Personal belongings that should not be given under any circumstances, even to close relatives Whether to give clothes to vilify a friend's child
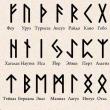
- Runa Dagaz: the meaning of the symbol and the photo Becoming "Happy pregnancy" from the Trap
- Remove generic damage on the maternal side
Advertising
| GCS - what is it in medicine? Action and effects of glucocorticosteroid preparations. Glucocorticosteroids Mast cell membrane stabilizers |
|
Excipients: dispersed cellulose (microcrystalline cellulose treated with sodium carmellose) - 20 mg, glycerol - 21 mg, citric acid monohydrate - 2 mg, sodium citrate dihydrate - 2.8 mg, polysorbate 80 - 0.1 mg, (in the form of a 50% solution) - 0.2 mg, purified water - 950 mg. 60 doses (10 g) - polyethylene bottles (1) complete with a dosing device - cardboard packs. pharmachologic effectGCS for local use. It has anti-inflammatory and effect when used in doses that do not cause systemic effects. It inhibits the release of inflammatory mediators. It increases the production of lipomodulin, which is an inhibitor of phospholipase A, which causes a decrease in the release of arachidonic acid and, accordingly, inhibition of the synthesis of metabolic products of arachidonic acid - cyclic endoperoxides, prostaglandins. Prevents marginal accumulation of neutrophils, which reduces inflammatory exudate and production of lymphokines, inhibits the migration of macrophages, and leads to a decrease in the processes of infiltration and granulation. Reduces inflammation by reducing the formation of chemotaxis substance (effect on late allergy reactions), inhibits the development of an immediate type of allergic reaction (due to inhibition of the production of metabolites of arachidonic acid and a decrease in the release of inflammatory mediators from mast cells). In studies with provocative tests with the application of antigens to the nasal mucosa, a high anti-inflammatory activity of mometasone was demonstrated, both in the early and in the late stages of an allergic reaction. This was confirmed by a decrease (compared with placebo) in the concentration of histamine and eosinophil activity, as well as a decrease (compared to baseline) in the number of eosinophils, neutrophils and epithelial cell adhesion proteins. PharmacokineticsSuction With intranasal administration, the systemic bioavailability of mometasone furoate is<1% (при чувствительности метода определения 0.25 пг/мл). Mometasone is very poorly absorbed from the gastrointestinal tract. Metabolism and excretion A small amount of active substance that can enter the gastrointestinal tract after intranasal administration is actively metabolized during the "first pass" through the liver. It is excreted in urine and bile. Indications- seasonal and year-round allergic rhinitis in adults, adolescents and children from 2 years of age; - acute sinusitis or exacerbation of chronic sinusitis in adults (including the elderly) and adolescents from the age of 12 - as an auxiliary therapeutic agent in antibiotic treatment; - acute rhinosinusitis with mild to moderate symptoms without signs of severe bacterial infection in patients aged 12 years and older; - prevention of moderate and severe seasonal allergic rhinitis in adults and adolescents from the age of 12 (it is recommended to carry out 2-4 weeks before the expected start of the dusting season); - polyposis of the nose, accompanied by impaired nasal breathing and smell in adults (over 18 years old). Contraindications- hypersensitivity to drug components; - recent surgery or nasal trauma with damage to the nasal mucosa - before the wound heals (due to the inhibitory effect of GCS on the healing process); - children and adolescents (with seasonal and year-round allergic rhinitis - up to 2 years, with acute sinusitis or exacerbation of chronic sinusitis - up to 12 years, with polyposis - up to 18 years) - due to the lack of relevant data; FROM caution the drug should be used in case of tuberculosis infection (active or latent) of the respiratory tract, untreated fungal, bacterial, systemic viral infection or infection caused by Herpes simplex with eye damage (as an exception, it is possible to prescribe the drug for these infections as directed by a doctor), the presence of untreated local infection with the involvement of the nasal mucosa in the process. DosageThe drug is administered intranasally. Treating seasonal or perennial allergic rhinitis The recommended prophylactic and therapeutic dose of the drug is 2 inhalations (50 mcg each) in each nostril 1 time / day (total daily dose - 200 mcg). Upon reaching the therapeutic effect for maintenance therapy, it is possible to reduce the dose to 1 inhalation in each nostril 1 time / day (total daily dose - 100 μg). If a decrease in the symptoms of the disease cannot be achieved by using the drug in the recommended therapeutic dose, the daily dose can be increased to 4 inhalations in each nostril 1 time / day (total daily dose - 400 μg). After reducing the symptoms of the disease, a dose reduction is recommended. The onset of action of the drug is usually noted clinically within 12 hours after the first use of the drug. Children aged 2-11 For the use of the drug in young children, adult assistance is required. Adjunctive treatment of acute sinusitis or exacerbation of chronic sinusitis Adults (including elderly patients) and adolescents from 12 years old If a decrease in the symptoms of the disease cannot be achieved by using the drug at the recommended therapeutic dose, the daily dose can be increased to 4 inhalations in each nostril 2 times / day (total daily dose - 800 mcg). After reducing the symptoms of the disease, a dose reduction is recommended Treating acute rhinosinusitis without evidence of severe bacterial infection Recommended dose for adults and adolescents is 2 inhalations of 50 mcg in each nasal passage 2 times / day (total daily dose of 400 mcg). If symptoms worsen during treatment, consult a specialist. Treatment of nasal polyposis For adults (including elderly patients) from 18 years the recommended therapeutic dose is 2 inhalations (50 mcg each) in each nostril 2 times / day (total daily dose - 400 mcg). Rules for using the drug Nasonex Inhalation of the suspension contained in the spray bottle is carried out using a special dispensing nozzle on the bottle. Before the first use of Nasonex nasal spray, it is necessary to calibrate by pressing the dosing device 10 times, until splashes appear, which indicates that the drug is ready for use. You should tilt your head and inject the drug into each nostril as recommended by your doctor. If the nasal spray has not been used for 14 days or longer, you must press the dispensing nozzle 2 times until a splash appears. Shake the bottle vigorously before each use. Cleaning the dispensing tip It is important to clean the dispensing tip regularly to avoid malfunctioning. Remove the dust cap on the nozzle, then carefully remove the spray tip. Thoroughly rinse spray tip and dust cap in warm water and rinse under tap. Do not try to open the nasal applicator with a needle or other sharp object, as this will damage the applicator and may result in an incorrect dose of the drug. Dry the cap and tip in a warm place. After that, you need to attach the spray tip to the bottle and screw the cap back to the bottle to protect it from dust. When using the nasal spray for the first time after cleaning, recalibrate by pressing the dispensing tip 2 times. Side effectsAdults and adolescents Adverse events associated with the use of the drug (\u003e 1%), identified during clinical trials in patients with allergic rhinitis or nasal polyposis, and during the period of post-registration use of the drug, regardless of the indication for use, are presented in Table 1. Adverse reactions are listed in accordance with with the classification of system-organ classes MedDRA. Within each system-organ class, adverse reactions are classified by frequency of occurrence. Nasal bleeding, as a rule, was moderate and stopped on its own, the frequency of their occurrence was slightly higher than with placebo (5%), but equal or less than with the appointment of other intranasal corticosteroids, which were used as active control (in some of the the incidence of nosebleeds was up to 15%). The incidence of all other adverse events was comparable to the incidence with placebo. * revealed with a frequency of "rare" when using the drug 2 times / day for nasal polyposis ** detected when using the drug 2 times / day with nasal polyposis Children Respiratory, chest and mediastinal disorders:nosebleeds (6%), irritation of the nasal mucosa (2%), sneezing (2%). Nervous system disorders:headache (3%). The incidence of these adverse events in children was comparable to the incidence of these adverse events with placebo. With the use of intranasal corticosteroids, systemic side effects may develop, especially with prolonged use of intranasal corticosteroids in high doses (see section "Special instructions"). OverdoseWith prolonged use of corticosteroids in high doses or with the simultaneous use of several corticosteroids, the hypothalamic-pituitary-adrenal system may be suppressed. The drug has a low systemic bioavailability (<1%, при чувствительности метода определения 0.25 пг/мл), поэтому маловероятно, что при случайной или намеренной передозировке потребуется принятие каких-либо специальных мер, кроме наблюдения с возможным последующим возобновлением приема препарата в рекомендованной дозе. Drug interactionsThe combination therapy was well tolerated by patients. At the same time, no effect of the drug on the concentration of loratadine or its main metabolite in blood plasma was noted. In these studies, mometasone furoate was not detected in the blood (with a sensitivity of the method for determining 50 pg / ml). special instructionsAs with any long-term treatment, patients who have been using Nasonex nasal spray for several months or longer should periodically see a doctor for possible changes in the nasal mucosa. It is necessary to monitor patients receiving intranasal corticosteroids for a long time. Development of growth retardation in children is possible. In case of detection of growth retardation in children, it is necessary to reduce the dose of intranasal corticosteroids to the lowest that allows effective control of symptoms. In addition, the patient should be referred to a pediatrician for consultation. If a local fungal infection of the nose or throat develops, it may be necessary to discontinue therapy with Nasonex nasal spray and carry out special treatment. Persistent irritation of the nasal mucosa and pharynx for a long time may also serve as a reason for discontinuing treatment with Nasonex nasal spray. When conducting placebo-controlled clinical studies in children, when Nasonex nasal spray was used in a daily dose of 100 mcg for a year, no growth retardation was observed in children. With prolonged treatment with Nasonex nasal spray, no signs of suppression of the function of the hypothalamic-pituitary-adrenal system were observed. Patients who switch to treatment with Nasonex nasal spray after prolonged therapy with systemic corticosteroids require special attention. Cancellation of systemic corticosteroids in such patients can lead to adrenal insufficiency, the subsequent recovery of which can take up to several months. If signs of adrenal insufficiency appear, you should resume taking systemic corticosteroids and take other necessary measures. With the use of intranasal corticosteroids, systemic side effects may develop, especially with prolonged use in high doses. The likelihood of developing these effects is much less than with the use of oral GCS. Systemic side effects may differ both in individual patients and depending on the GCS used. Potential systemic effects include Cushing's syndrome, characteristic features of Cushingoid, adrenal suppression, growth retardation in children and adolescents, cataracts, glaucoma, and less commonly a range of psychological or behavioral effects, including psychomotor hyperactivity, sleep disturbance, anxiety, depression, or aggression (especially in children). During the transition from treatment with systemic corticosteroids to treatment with nasal spray Nasonex, some patients may experience initial symptoms of cancellation of systemic corticosteroids (for example, pain in joints and / or muscles, fatigue and depression), despite a decrease in the severity of symptoms associated with mucosal damage shell of the nose. Such patients must be specially convinced of the advisability of continuing treatment with Nasonex nasal spray. The transition from systemic to local corticosteroids can also reveal allergic diseases, such as allergic conjunctivitis and eczema, that already existed, but were masked by systemic corticosteroids therapy. Patients undergoing treatment with GCS have a potentially reduced immune reactivity and should be warned about the increased risk of infection for them in case of contact with patients with certain infectious diseases (for example, chickenpox, measles), as well as the need for medical advice if such contact occurs ... If signs of severe bacterial infection appear (for example, fever, persistent and sharp pain on one side of the face or toothache, swelling in the orbital or periorbital region), immediate medical advice is required. When using the nasal spray Nasonex for 12 months, there were no signs of atrophy of the nasal mucosa. In addition, mometasone furoate showed a tendency to contribute to the normalization of the histological picture in the study of biopsies of the nasal mucosa. The efficacy and safety of mometasone has not been studied in the treatment of unilateral polyps, polyps associated with cystic fibrosis, and polyps that completely obstruct the nasal cavity. If unilateral polyps of an unusual or irregular shape are detected, especially ulcerated or bleeding polyps, additional medical examination is necessary. Influence on the ability to drive vehicles and work with mechanisms There is no data on the effect of Nasonex on the ability to drive a car or move machinery. Pregnancy and lactationThere have been no special, well-controlled studies of the safety of Nasonex during pregnancy. Like other GCS for intranasal use, Nasonex should be prescribed during pregnancy and during breastfeeding only if the expected benefit from its use justifies the potential risk to the fetus or infant. Infants whose mothers received GCS during pregnancy should be carefully examined to detect possible adrenal hypofunction. Childhood useContraindicated in seasonal and year-round allergic rhinitis - in children under 2 years of age, with acute sinusitis or exacerbation of chronic sinusitis - up to 12 years, with polyposis - up to 18 years (due to lack of relevant data). When conducting placebo-controlled clinical studies in children, when Nasonex was used at a dose of 100 μg / day for a year, no growth retardation was observed. For violations of liver functionA small amount of the active substance, which can enter the gastrointestinal tract during intranasal administration, is absorbed to an insignificant extent and is actively biotransformed during the "first pass" through the liver. Terms of dispensing from pharmaciesThe drug is available by prescription. Storage conditions and periodsThe drug should be stored out of the reach of children at a temperature of 2 ° to 25 ° C. Do not freeze. Shelf life is 2 years. E.A. Ushkalova, Professor, Department of General and Clinical Pharmacology, PFUR, Moscow Allergic rhinitis is one of the most common diseases, the prevalence and frequency of which continues to grow at an extremely high rate. So, over the past 30 years, during each decade, the incidence in economically developed countries has increased by 100%, which made it possible to call it epidemic. According to epidemiological studies, the prevalence of allergic rhinitis is on average 10-25% in the world, in Europe - 20-30, in New Zealand and Australia - about 40, in South Africa - about 17, in Russia - 25%. In the United States, allergic rhinitis affects about 40 million people annually, including about 10-30% of the adult population and 40% of children. In 80% of cases, the disease begins before the age of 20. In Russia, according to official statistics, allergic rhinitis occurs in 9-25% of children 5-8 years old. However, according to Russian and foreign experts, the official data on the incidence rate, based on the referral of patients, in no way reflects the true prevalence of allergic rhinitis, since they do not take into account the huge number of people who did not seek medical help and patients who were given wrong diagnosis. There is information that in Europe, including Russia, no more than 60% of patients seek medical help for symptoms of allergic rhinitis. According to the results of a survey of 1000 patients conducted in the clinic of the State Scientific Center - Institute of Immunology of the Ministry of Health of Russia, only 12% of patients are diagnosed with allergic rhinitis in the first year of the disease, 50% - in the first five years, the rest - 9-30 years or more after the onset of symptoms. The direct medical costs of allergic rhinitis in the United States are estimated at $ 4.5 billion per year. The indirect costs associated with the loss of 3.8 million workers and 2 million academic days further add to the cost of the disease to the health system and society at large. The clinical and economic burden of allergic rhinitis is also due to a decrease in the quality of life of patients, as well as the risk of developing serious complications from the respiratory tract and ENT organs. In particular, allergic rhinitis is considered a risk factor for the development of bronchial asthma. It occurs in 80-90% of patients with bronchial asthma, and in 68% of children with allergic rhinitis, bronchial hyperreactivity is detected. The close relationship between bronchial asthma and allergic rhinitis allows some authors to consider them as a single disease. Allergic rhinitis is also often associated with sinusitis, conjunctivitis, otitis media, pharyngitis, laryngitis, snoring, and sleep apnea. Some studies have found an association of allergic rhinitis with depression and lower back pain. Thus, the treatment of allergic rhinitis and the prevention of concomitant diseases are of great medical, social and economic importance. Allergic rhinitis treatment methods Treatment of patients with allergic rhinitis includes non-pharmacological and pharmacological methods. The first are primarily aimed at eliminating allergens and provoking factors or reducing contact with them. In most cases, complete elimination of the allergen is not possible, especially in patients with perennial (persistent) rhinitis who are constantly exposed to it. In many situations, effective elimination of allergens is impossible not only for practical, but also for economic reasons, as it is associated with significant financial costs for the patient. However, even reducing exposure to the allergen can improve symptom control and reduce the need for pharmacotherapy. In numerous clinical studies, the effectiveness of specific immunotherapy in allergic rhinitis has been proven, but this method of treatment is also not without a number of disadvantages. First, specific immunotherapy is effective only in patients with hypersensitivity to a limited spectrum (1 or 2) of allergens. Secondly, high efficiency (80-90%) is shown in clinical trials only when parenteral specific immunotherapy is used, which is not very convenient for patients, since it is a slow gradual process of subcutaneous administration of antigen in increasing doses. In addition, it is expensive and unsafe, as it can cause life-threatening anaphylactic reactions. Routine use of the more convenient sublingual immunotherapy based on the analysis of 23 placebo-controlled double-blind studies cannot be recommended at this time. In addition, the doses of the allergen required for sublingual immunotherapy are 5-200 times higher than those for parenteral. In view of the above, foreign experts recommend reserving immunotherapy for patients with severe disrupting daily life symptoms, whose disease is caused by a limited number of identified allergens and who do not respond to treatment with other methods. Thus, the main place in the prevention and treatment of allergic rhinitis belongs to drugs. For this purpose, drugs of several pharmacological groups are used: blockers of H1-histamine receptors, corticosteroids, stabilizers of mast cell membranes, vasoconstrictors (decongestants), M-anticholinergics. The effectiveness of drugs in this disease and relatively new groups - antagonists of leukotriene receptors and monoclonal antibodies is being studied. One of the leukotriene antagonists, montelukast, was recently approved for the treatment of seasonal allergic rhinitis. In general, all drugs used to treat allergic rhinitis can be divided into two groups: 1) drugs that control the symptoms of the disease, and 2) drugs that act on pathogenetic factors, that is, they have a truly therapeutic effect. The latter group primarily includes corticosteroids, the importance of which has sharply increased after their introduction into medical practice in the early 1970s. the first drug in this group (beclomethasone dipropionate) for intranasal use. The place of intranasal corticosteroids in the treatment of allergic rhinitis Despite the fact that glucocorticoids have been used for the treatment of diseases of the upper respiratory tract for more than a century, their mechanism of action continues to be actively studied. Experimental and clinical studies have shown that glucocorticoids affect almost all stages of the pathogenesis of allergic rhinitis. Their therapeutic effect in allergic rhinitis is associated primarily with anti-inflammatory and desensitizing effects. It has been established that glucocorticoids inhibit the synthesis of a number of cytokines, in particular IL-1, IL-3, IL-4, IL-5, IL-6, IL-13, TNF-a and GM-CSF. In addition, they reduce the induction of nitric oxide (NO) synthetase, the activation of which leads to excess production of NO, which has a pronounced pro-inflammatory effect. Glucocorticoids also reduce the activity of genes encoding the synthesis of enzymes involved in the production of other pro-inflammatory protein molecules: cyclooxygenase, phospholipase A2 and endothelin-1, and inhibit the expression of adhesion molecules: ICAM-1 and E-selectin. At the cellular level, glucocorticoids cause a decrease in the number of mast cells, basophils and the mediators they release; reduce the number of eosinophils and their products in the epithelium and in its own layer of the mucous membrane. They also influence the processes of apoptosis, reducing the lifespan of eosinophils; reduce the number of Langerhans cells and inhibit the capture and transport of antigens by these cells; reduce the number of T cells in the epithelium; reduce the production of leukotrienes in the mucous membrane; inhibit IgE production. Glucocorticoids reduce mucosal glandular secretion, plasma extravasation and tissue edema. In addition, they reduce the sensitivity of the receptors of the nasal mucosa to histamine and mechanical stimuli, i.e., to a certain extent, they also affect nonspecific nasal hyperreactivity. The impact on all links of the pathogenesis of the disease and the inhibition of both early and delayed phases of an allergic reaction is characteristic not only of systemic glucocorticoids, but also of intranasal drugs of this group. The advantage of intranasal glucocorticoids over oral ones is the minimal risk of systemic side effects against the background of the creation of adequate concentrations of the active substance in the nasal mucosa, which makes it possible to control the symptoms of allergic rhinitis. Intranasal corticosteroids have been shown to be effective in both preventing and alleviating symptoms associated with the early and late phases of the allergic response. A decrease in the number of T-lymphocytes, eosinophils, basophils, monocytes and mast cells in the upper respiratory tract under their influence causes a decrease in nasal congestion, rhinorrhea, sneezing and itching, which leads to a significant improvement in the quality of life of patients. Several studies have shown that intranasal glucocorticoids can almost completely prevent the symptoms of the late phase of the allergic response. Comparative characteristics of intranasal corticosteroids and other drugs widely used for the treatment of allergic rhinitis are presented in table. 1, which shows that intranasal corticosteroids relieve symptoms of the disease to a greater extent than drugs of all other groups. The results of clinical studies and meta-analyzes allow them to be considered the most effective agents for the treatment of allergic rhinitis and to be considered as first-line drugs for this disease. Table 1. Comparative characteristics of corticosteroids and other drugs for the treatment of allergic rhinitis
In international clinical practice, the following intranasal corticosteroids are currently widely used: triamcinolone acetonide, beclamethasone dipropionate, flunisolide, budesonide, fluticasone propionate and mometasone furoate. In Russia, flunisolide and triamcinolone in the form of nasal aerosols are not used. The use of hydrocortisone and prednisolone intranasally is not rational, since these drugs have a very high bioavailability and can cause systemic side effects, especially when sprayed into the nasal cavity. Due to the high bioavailability, intranasal dosage forms of dexamethasone and betamethasone also lose their practical value. In contrast, modern intranasal glucocorticoids have low bioavailability (Table 2) and are well tolerated by patients. It should be borne in mind that the bioavailability of intranasal drugs is determined not only by their absorption from the nasal mucosa, but also by the absorption of that part of the dose (less than half of the administered dose), which, having settled in the pharynx, is swallowed and absorbed in the intestine. In addition, with a normally functioning mucociliary transport, the main part of the drug (up to 96%) within 20-30 minutes after intranasal administration is transferred to the pharynx using the cilia of the nasal mucosa, from where it enters the gastrointestinal tract and is absorbed. Therefore, oral and intranasal bioavailability is an important characteristic of intranasal corticosteroids, which largely determines their therapeutic index, that is, the ratio of local anti-inflammatory activity and potential for adverse systemic action. Table 2. Bioavailability of intranasal corticosteroids The low bioavailability of modern intranasal corticosteroids is associated not only with their poor absorption, but also with a rapid and almost complete metabolism during the first passage through the liver. This leads to a generally short half-life of intranasal corticosteroids, but its duration is different for different drugs. Intranasal corticosteroids also differ in the degree of lipophilicity, which determines the volume of their distribution in the body, in the degree of affinity for the receptors and in the potency. To measure the strength of the action of topical corticosteroids, 2 methods are used - determining the degree of affinity for glucocorticoid receptors and vasoconstrictor activity on a skin model. According to the degree of affinity for the receptors, the drugs are arranged in the following ascending order: dexamethasone, triamcinolone acetonide, budesonide, fluticasone propionate and mometasone furoate. Fluticasone propionate and mometasone furoate are superior to other intranasal drugs in terms of vasoconstrictor activity. However, vasoconstrictor activity only partially determines the effectiveness of corticosteroids in allergic rhinitis, since it does not directly correlate with anti-inflammatory activity. Drugs with high lipophilicity, such as fluticasone propionate or mometasone furoate, penetrate tissues better and have a large volume of distribution in them. They can create a reservoir in the tissues from which the active substance is slowly released, resulting in a significantly longer terminal half-life from the body. In contrast, less lipophilic corticosteroids, such as triamzionolone acetonide or budesonide, have a lower volume of distribution. A high degree of lipophilicity reduces the water solubility of drugs in the mucous membrane and, thus, increases the amount of active substance excreted by mucociliary clearance even before it reaches the receptor in the tissues. This can help reduce the local anti-inflammatory activity of the drug in the nose, but at the same time, reduce its absorption from the mucous membrane into the systemic circulation. The clinical significance of high lipophilicity requires further study. The onset of the therapeutic effect of intranasal glucocorticoids is usually observed several days after the first administration (Table 3), but it may take several weeks to achieve the maximum effect. Table 3. Onset of action of intranasal corticosteroids The efficacy and tolerability of intranasal corticosteroids is largely determined by their delivery system into the nasal cavity. The most widely used dosage forms are metered-dose aerosols and nasal sprays. The latter provide a more efficient delivery of the active substance and less often cause local side effects (nosebleeds, dryness, burning in the nose, itching, sneezing), which, when dosed aerosols are used, are largely due to the irritating effect of freon and the high rate of drug entry into the nasal cavity. The effectiveness of modern intranasal corticosteroids in allergic rhinitis has been proven in numerous placebo-controlled studies and comparative studies with drugs from other pharmacological groups. Thus, in three meta-analyzes of randomized controlled trials, it was shown that intranasal corticosteroids are significantly superior in their ability to eliminate sneezing, rhinorrhea, itching, nasal congestion and impairment of smell, topical and oral antihistamines, including drugs of the latest generations. In a randomized clinical trial in patients with allergic rhinitis, intranasal budesonide monotherapy (200 mcg) was equally effective with the combination of an antihistamine (cetirzine, 10 mg) and a leukotriene antagonist (montelukast, 10 mg) for nasal congestion and improved nasal breathing. Moreover, analysis of published data suggests that intranasal corticosteroids are significantly more effective in relieving symptoms of allergic rhinitis than antihistamines, leukotriene antagonists, and combinations thereof. According to international recommendations (the WHO ARIA program - Allergic rhinitis and its impact on asthma), intranasal corticosteroids can be used at all stages of allergic rhinitis, from mild forms of intermittent (seasonal) to severe forms of persistent (year-round), and with moderate and severe course of the disease they are considered as the first choice. Along with improving the symptoms of allergic rhinitis and influencing the pathogenetic mechanisms of the disease, intranasal corticosteroids play an important role in the treatment of concomitant diseases such as bronchial asthma, sinusitis and nasal polyps. Despite the differences in the physicochemical, pharmacodynamic and pharmacokinetic properties of topical glucocorticoids, most comparative clinical studies have failed to demonstrate the therapeutic benefits of some drugs over others. For example, in a comparative study of budesonide (400 mcg 1 r / day) and mometasone furoate (200 mcg 1 r / day), despite the above-mentioned pharmacodynamic and pharmacokinetic advantages of the latter, the equal effectiveness of both drugs in preventing symptoms of seasonal allergic rhinitis was shown, which was estimated by the number of days elapsed from the beginning of the allergic season to the onset of relatively severe symptoms of the disease. Both drugs were significantly superior in this indicator to placebo: when using mometasone, symptoms occurred on average after 26 days, budesonide - 34 days, placebo - 9 days. Moreover, in another study, in patients with perennial rhinitis, budesonide (256 μg 1 r / day) was significantly superior in the effectiveness of eliminating all symptoms, as well as in the effectiveness of eliminating nasal congestion, another drug with low bioavailability and high affinity for glucocorticoid receptors - fluticasone ( 200 mcg 1 r / day). Perhaps this is due to the ability of the drug to undergo esterification, which is associated with the prolongation of its anti-inflammatory action in comparison with corticosteroids that do not form esters, in particular fluticasone. In clinical studies, it was confirmed that 6 hours after administration, the concentration of budesonide, according to nasal biopsy, exceeded the concentration of fluticasone propionate by more than 10 times, and after 24 hours - more than three times. The authors of the review devoted to this issue suggest that due to this mechanism, the ratio of local benefit and systemic risk may shift for the better in budesonide due to the lower systemic formation of esters compared to their formation in the respiratory tract. However, this issue requires further study. According to the meta-analysis, all topical corticosteroids in all intranasal dosage forms are effective and safe agents that significantly improve the quality of life of patients. Nevertheless, targeted studies have shown that the organoleptic properties and dosage forms of drugs have a pronounced effect on patient preferences and, consequently, on the accuracy of their compliance with the prescribed treatment regimen. Thus, in one study of patient preferences, in which 503 patients and 100 doctors participated, it was shown that 97% of patients prefer nasal sprays devoid of "aftertaste" and / or odor. According to the results of this study, 97% of physicians are confident that the organoleptic properties of intranasal corticosteroids affect patients' adherence to treatment, but in actual practice, more than half of them do not ask the patient about their preferences when prescribing a drug. Another multicenter, randomized, blinded study compared the preference of patients with mild to moderate allergic rhinitis for budesonide nasal spray and fluticasone propionate nasal spray. The sensory perception of the budesonide spray by the patients was significantly superior to that of the fluticasone spray in various respects, and therefore most patients preferred the budesonide spray. In another placebo-controlled study, which compared intranasal dosage forms of the same drugs in patients with seasonal allergic rhinitis, despite the equal clinical efficacy of budesonide and fluticasone, patients' quality of life improved more in the budesonide group. Thus, the ability of intranasal corticosteroids to affect all the symptoms of allergic rhinitis, including nasal congestion and impaired smell, distinguishes them favorably from drugs of other pharmacological groups, especially in persistent (year-round) rhinitis, when difficulty in nasal breathing is the main symptom. All modern drugs in this group are effective and safe. Treatment regimens with modern intranasal corticosteroids are presented in table. 4. The duration of the course of treatment depends on the severity of rhinitis and can range from 10 days to 3 months. The choice of a particular drug is determined mainly by the price and preferences of the patients. Both of these factors can have a significant impact on treatment adherence and therapy effectiveness. Table 4. Schemes of intranasal corticosteroid administration * The drug "Benarin" 30 mcg in each nostril 2 r / day. literature: Aberg N, Sundell J, Eriksson B, Hesselmar B, Aberg B. Prevalence of allergic disease in schoolchildren in relation to family history, upper respiratory tract infections, and residential characteristics. Allergy. 1996; 51: 232-237. Sibbald B, Rink E, D'Souza M. Is the prevalence of atopy increasing? Br J Gen Pract. 1990; 40: 338-340. Ceuppens J. Western lifestyle, local defenses and the rising incidence of allergic rhinitis. Acta Otorhinolaryngol Belg. 2000; 54: 391-395. Ilyina N.I., Polner S.A. Year-round allergic rhinitis // Consilium medicum. 2001. T. 3. No. 8. S. 384-393. L.V. Luss Allergic rhinitis: problems, diagnosis, therapy // Attending physician. 2002. No. 4. S. 24-28. Pytsky V.I. and other Allergic diseases. M .: Triada-X, 1999.470 p. Patterson R. et al. Allergic diseases. M .: Geotar, 2000.733 p. Naclerio RM, Solomon W. Rhinitis and inhalant allergens. JAMA 1997; 278: 1842-8. GlaxoWellcome. The health and economic impact of rhinitis. Am J Manag Care 1997; 3: S8-18. Sibbald B. Epidemiology of allergic rhinitis. In: ML B, ed. Epidemiology of Clinical Allergy. Monographs in Allergy. Basel, Switzerland: Karger; 1993: 61-69. Geppe N.A. Possibilities of using antihistamines in pediatric practice // Selected lectures for practicing doctors. IX Russian National Congress "Man and Medicine". M., 2002.S. 250-261. Khaitov R.M., Bogova A.V., Ilyina N.I. Epidemiology of allergic diseases in Russia // Immunology. 1998. No. 3. S. 4-9. Ilyina N.I. Allergic pathology in different regions of Russia based on the results of clinical and epidemiological studies: Author's abstract. doct. diss. M., 1996.24 p. Dykewicz MS, Fineman S, Skoner DP, et al. Diagnosis and management of rhinitis: complete guidelines of the Joint Task Force on Practice Parameters in Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 1998; 81 (5 Pt 2): 478-518. American Academy of Allergy, Asthma, and Immunology. The allergy report. Milwaukee: American Academy of Allergy, Asthma, and Immunology, 2000. Bousquet J, van Cauwenberge P, Khaltaev N. et al. Allergic rhinitis and its impact on asthma (ARIA) - Pocket Guide. - WHO. 2001; 23: 5. Studenikina N.I., Revyakina V.A., Lukina O.F., Kulichenko T.V. Problems of early detection, prevention and therapy of atopic diseases in children // Coll. of theses of the 1st All-Russian Congress on Pediatric Allergology. M., November 29-30, 2001, p. 144. Coste A. ENT diseases associated with allergic rhinitis: a review of the literature. Ann Otolaryngol Chir Cervicofac. 2000; 117: 168-173. Hurwitz EL, Morgenstern H. Cross-sectional associations of asthma, hay fever, and other allergies with major depression and low-back pain among adults aged 20-39 years in the United States. Am J Epidemiol. 1999; 150: 1107-1116. Trangsrud AJ, Whitaker AL, Small RE. Intranasal Corticosteroids for Allergic Rhinitis. Pharmacotherapy 22 (11): 1458-1467, 2002. A.S. Lopatin Algorithms for the diagnosis and treatment of allergic and vasomotor rhinitis // RMZh. 2002. T. 10.No. 17. Malling HJ. Immunotherapy as an effective tool in allergy treatment. Allergy. 1998 May; 53 (5): 461-72. Varney VA, Edwards J, Tabbah K, Brewster H, Mavroleon G, Frew AJ. Clinical efficacy of specific immunotherapy to cat dander: a double-blind placebo-controlled trial. Clin Exp Allergy. 1997 Aug; 27 (8): 860-7. Durham SR, Ying S, Varney VA, et al. Cytokine messenger RNA expression for IL-3, IL-4, IL-5 and GM-CSF in the nasal mucosa after local allergen provocation: relationship to tissue eosinophilia. J Immunol 1992; 148: 2390-4. Anonymous. Guidelines to minimize the risk from systemic reaction caused by immunotherapy with allergen extracts. J Allergy Clin Immunol 1994; 93 (5): 811-12. Malling H-J. Is Sublingual Immunotherapy Clinically Effective? Curr Opin Allergy Clin Immunol 2002; 2: 523-32. Guez S, Vatrinet C, Fadel R, Andre C. House-dust mite sublingual swallow immunotherapy (SLIT) in perennial rhinitis: a double-blind, placebo-controlled study. Allergy. 2000; 55: 369-375. Casale TB, Bernstein IL, Busse WW, et al. Use of an anti-IgE humanized monoclonal antibody in ragweed-induced allergic rhinitis. J Allergy Clin Immunol 1997; 100: 110-21. Shields RL, Whether WR, Zioncheck K, et al. Inhibition of allergic reactions with antibodies to IgE. Int Arch Allergy Immunol 1995; 7: 308-12. Philip G, Malmstrom K, Hampel FC Jr, et al. Montelukast for treating seasonal allergic rhinitis: a randomized, double-blind, placebo-controlled trial performed in the spring. Clin Exp Allergy. 2002; 32: 1020-1028. Nathan RA. Pharmacotherapy for allergic rhinitis: a critical review of leukotriene receptor antagonists compared with other treatments. Ann Allergy Asthma Immunol. 2003; 90: 182-191. A.S. Lopatin Corticosteroid therapy in the treatment of diseases of the nose and paranasal sinuses: historical aspects // Consilium-medicum. 2004. T. 6. No. 4. Mygind N, Nielsen LP, Hoffmann HJ, et al. Mode of action of intranasal corticosteroids. J Allergy Clin Immunol 2001; 108 (suppl 1): S16-25. Mygind N, Dahl R. The rationale for use of topical corticosteroids in allergic rhinitis. Clin Exp Allergy 1996; 26 (suppl 3): 2-10. Mygind N. Glucocorticosteroids and rhinitis. Allergy 1993; 48: 476-90. Wiseman LR, Benfield P. Intranasal fluticasone propionate: a reappraisal of its pharmacology and clinical efficacy in the treatment of rhinitis. Drugs 1997; 53: 885-907. Onrust SV, Lamb HM. Mometasone furoate: a review of its intranasal use in allergic rhinitis. Drugs 1998; 56: 725-45. Gasbarro R. Identifying and managing patients with asthma and allergy. Drug Topics 2001; 7: 68-77. Tripathy A, Patterson R. Impact of allergic rhinitis treatment on quality of life. Pharmacoeconomics 2001; 19 (9): 891-9. Rak S, Jacobson MR, Suderick RM, et al. Influence of prolonged treatment with topical corticosteroid (fluticasone propionate) on early and late phase responses and cellular infiltration in the nasal mucosa after allergen challenge. Clin Exp Allergy 1994; 24 (10): 930-9. Konno A, Yamakoshi T, Terada N, Fujita Y. Mode of action of a topical steroid on immediate phase reaction after antigen challenge and nonspecific nasal hyperreactivity in nasal allergy. Int Arch Allergy Immunol 1994; 103 (1): 79-87. Corren J. Intranasal corticosteroids for allergic rhinitis: how do different agents compare? J Allergy Clin Immunol 1999; 104 (4): S144-9. Mabry RL. Pharmacotherapy of allergic rhinitis: corticosteroids. Otolaryngol Head Neck Surg 1995; 113: 120-5. Lund V. International rhinitis management working group. International consensus report on the diagnosis and management of rhinitis. Allergy 1994; 49 (suppl 19): 1-34. LaForce C. Use of nasal steroids in managing allergic rhinitis. J Allergy Clin Immunol 1999; 103: S388-94. Emelyanov A.V., Lukyanov S.V. Nasal glucocorticoids // Rational pharmacotherapy of respiratory diseases. M .: "Litter", 2004. S. 93-97. Smith CL, Kreutner W. In vitro glucocorticoid receptor binding and transcriptional activation by topically active glucocorticoids. Arzneimittelforschung / Drug Res 1998; 48: 956-60. Lipworth BJ, Jackson CM. Safety of inhaled and intranasal corticosteroids: lessons for the new millennium. Drug Saf. 2000 Jul; 23 (1): 11-33. Buck ML. Intranasal Steroids for Children With Allergic Rhinitis. Pediatr Pharm 7 (5), 2001. Yanez A, Rodrigo GJ. Intranasal corticosteroids versus topical H1 receptor antagonists for the treatment of allergic rhinitis: a systemic review with meta-analysis. Ann Allergy Asthma Immunol. 2002; 89: 479-484. Weiner JM, Abramson MJ, Puy RM. Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: systematic review of randomized controlled trials. BMJ. 1998; 317: 1624-1629. Stempel DA, Thomas M. Treatment of allergic rhinitis: an evidence-based evaluation of nasal corticosteroids versus nonsedating antihistamines. Am J Manag Care 1998; 4: 89-96. Wilson A., Orr L., Sims E., Dempsey O., Lipworth B. Antiasthmatic activity of combined oral histamine and leukotriene antagonism versus inhaled and intra-nasal corticosteroid in seasonal allergic rhinitis (SAR) and asthma // 56th An-nual Meeting. American Academy of Allergy Asthma & Immunology. 03-Mar-2000. Abs. 1078. San Diego. United States. Nelson HS. Advances in upper airway diseases and allergen immunotherapy. J Allergy Clin Immunol. 2003; 111: S793-S798. Stanaland BE. Treatment of Allergic Rhinitis and Its Comorbidities. June 24, 2003 http://www.medscape.com/viewprogram/2344_pnt Meltzer EO. Clinical and antiinflammatory effects of intranasal budesonide aqueous pump spray in the treatment of perennial allergic rhinitis. Ann Allergy Asthma Immunol 1998; 81: 128-34. Brannan MD, Herron JM, Affrime MB. Safety and tolerability of once-daily mometasone furoate aqueous nasal spray in children. Clin Therapeut 1997; 19: 1330-9. Meltzer EO, \u200b\u200bBerger WE, Berkowitz RB, et al. A dose-ranging study of mometasone furoate aqueous nasal spray in children with seasonal allergic rhinitis. J Allergy Clin Immunol 1999; 104: 107-14. Ngamphaiboon J, Thepchatri A, Chatchatee P, et al. Fluticasone propionate aqueous nasal spray treatment for perennial allergic rhinitis in children. Ann Allergy Asthma Immunol 1997; 78: 479-84. Fluticasone Propionate Collaborative Pediatric Working Group. Treatment of seasonal allergic rhinitis with once-daily intranasal fluticasone propionate therapy in children. J Pediatr 1994; 125: 628-34. Small P, Houle P, Day JH, et al. A comparison of triamcinolone acetonide nasal aqueous spray and fluticasone propionate aqueous solution spray in the treatment of spring allergic rhinitis. J Allergy Clin Immunol 1997; 100: 592-5. Mandl M, Nolop K, Lutsky BN, et al. Comparison of once daily mometasone furoate and fluticasone propionate aqueous nasal sprays for the treatment of perennial rhinitis. Ann Allergy Asthma Immunol 1997; 79: 237-45. Marazzi P, Nolop K, Lutsky BN, et al. Prophylactic use of once-daily mometasone furoate (Nasonex) aqueous nasal spray in patients with seasonal allergic rhinitis. J Allergy Clin Immunol 1997; 99: S440. Day J, Carrillo T. Comparison of the efficacy of budesonide and fluticasone propionate aqueous nasal spray for once daily treatment of perennial allergic rhinitis, J Allergy Clin Immunol 1998; 102: 902-8. Edsbacker S, Brattsand R. Budesonide fatty-acid esterification: a novel mechanism prolonging binding to airway tissue. Review of available data. Ann Allergy Asthma Immunol. 2002 Jun; 88 (6): 609-16. Kaliner MA. Patient preferences and satisfaction with prescribed nasal steroids for allergic rhinitis. Allergy Asthma Proc. 2001; 22 (6 suppl): S11-S15. Bachert C, EI-Akkad T. Patient preferences and sensory comparisons of three intranasal corticosteroids for the treatment of allergic rhinitis. Ann Allergy Asthma Immunol. 2002; 89: 292-297. Shah SR, Miller C, Pethick N, O'Dowd L. Patients with allergic rhinitis prefer budesonide aqueous nasal spray to fluticasone propionate nasal spray based on sensory attributes. Program and abstracts of the 58th Annual Meeting of the American Academy of Allergy, Asthma and Immunology; March 1-6, 2002; New York, NY. Ciprandi G, Canonica WG, Grosclaude M, Ostinelli J, Brazzola GG, Bousquet J. Effects of budesonide and fluticasone propionate in a placebo-controlled study on symptoms and quality of life in seasonal allergic rhinitis. Allergy. 2002; 57: 586-591. Corticoids are hormonal substances produced by the human adrenal cortex. There are several types of them - mineral and glucocorticoids. Preparations that contain only one type of the hormonal substances listed are called corticosteroids. Intranasal corticosteroids are the most commonly used form of these medications in otolaryngology.
Synthetic glucocorticoids have the same properties as natural ones. Nasal corticosteroids, like other forms of hormonal drugs, have pronounced anti-inflammatory and anti-allergic effects. The anti-inflammatory effect is based on the inhibition of the production of active substances (leukotrienes, prostaglandins), which take part in the protective function of the body. There is also a delay in the multiplication of new protective cells, which significantly affects local immunity. The antiallergic action of hormonal drugs is performed by inhibiting the release of allergy mediators, in particular, histamine. As a result, a long-term (throughout the day) anti-edema effect is achieved.
Nasal corticosteroid useCurrently, in the practice of an ENT doctor, the use of hormonal groups of drugs is widespread, based on their high efficiency. Most often they are prescribed for diseases that arise against the background of contact with an allergen:
Nasal corticosteroids effectively eliminate local allergic manifestations, namely sneezing, nasal congestion, rhinorrhea. Drugs are also prescribed for vasomotor rhinitis in pregnant women. In this situation, they significantly improve nasal breathing, but do not contribute to a complete cure. When polyps are detected in the nasal cavity, the use of nasal hormonal drugs, at the moment, has no alternative among other methods of drug treatment. Before using the nasal hormonal agent directly, it is important to establish the cause of the disease.
ContraindicationsIn most cases, taking glucocorticoid drugs is well tolerated by patients. Despite this, there are a number of restrictions on their purpose:
Taking hormonal drugs for pregnant women is prescribed with caution, and during breastfeeding they are not at all recommended for use. Side effectsThe most often undesirable clinical manifestations from the body occur during their prolonged and uncontrolled use. You can observe:
If corticosteroid drugs are used for a long time in high doses, the risk of developing candidiasis in the nasopharynx area increases.
Release forms
Intranasal hormonal drugs are available in the form of drops and sprays. It is necessary to instill the medicine in the nose in a supine position, with the head thrown back and laid aside for the best drug entry into the nasal cavity. If the technique of instilling the medicine is not followed, a person may experience painful sensations in the forehead, a sensation of a taste of the drug in the mouth. Unlike drops, nasal sprays are much more convenient to use because they do not require any preparation before applying them. Their main advantage is that due to the presence of the dispenser, it is difficult to overdose the drug. Types of intranasal hormonal drugsCurrently, on the pharmaceutical market there are a large number of hormonal drugs that are similar in their effect, but have a different degree of pronounced effectiveness. The table below shows the most common nasal corticosteroid medications and their analogues.
It is worth dwelling on the features of the main drugs in order to understand what the advantage of each of them is. Fliksonase In addition to the main substance - fluticasone propionate, the drug contains a number of auxiliary components: dextrose, cellulose, phenylethyl alcohol and purified water. Fliksonase is produced in bottles with a dispenser for 60 and 120 doses (in one dose - 50 μg of active substance). The anti-inflammatory effect of the drug is moderately pronounced, but it has a fairly strong antiallergic property. The clinical effect of the drug develops 4 hours after administration, but a significant improvement in the condition occurs only 3 days from the start of therapy. If the symptoms of the disease decrease, the dosage can be reduced. The average course duration is 5-7 days. Allowed to take the drug for prophylactic purposes during seasonal allergies. Unlike other hormonal drugs, Fliksonase does not have a negative effect on the hypothalamic-pituitary system.
Alcedeen
The drug is available in 8.5 g cylinders with a dispenser and a mouthpiece in the form of a white, opaque suspension. Contains the active substance - beclomethasone (in one dose - 50 mcg). In addition to anti-inflammatory, antiallergic, it also exhibits immunosuppressive effects. When using standard doses, the drug does not have a systemic effect. When injecting Alsedin into the nasal cavity, avoid direct contact of the applicator with the mucous membrane. Rinse your mouth after each dose. In addition to indications for use common with other hormonal agents, it can be used as part of the complex therapy of bronchial asthma (not used during an attack). Alcedine can increase blood glucose, so it should be taken with caution by people with diabetes. Also, special attention during its reception is paid to people with hypertension, with impaired function of the liver and thyroid gland. For women in the first trimester of pregnancy and during breastfeeding, as well as for children under 6 years of age, the drug is contraindicated. Nazonex
The main component of the drug is mometasone furoate, a synthetic glucocorticosteroid with pronounced anti-inflammatory and antihistamine effects. It is produced in the form of a white suspension in plastic bottles with a volume of 60 and 120 doses. In its action and method of application, Nasonex is similar to Fliksonase, but, unlike it, has an effect on the hypothalamic-pituitary system. The first clinical effect after the administration of the drug is observed after 12 hours, which is significantly later than when taking Fliksonase. Very rarely, prolonged and uncontrolled administration of a drug can lead to an increase in intraocular pressure and a violation of the integrity of the nasal septum (its perforation). Nasonex is not prescribed for people with pulmonary tuberculosis, for acute infectious diseases, as well as for people who have recently undergone trauma or surgery in the nasopharynx. There are no absolute contraindications to taking this drug in pregnant women.
AvamisA hormonal drug in which, unlike others, a powerful anti-inflammatory effect prevails. It contains fluticasone furoate and excipients. It is produced, like the previous drugs, in vials with a volume of 30, 60 and 120 doses. The clinical effect after the first dose becomes noticeable after 8 hours. If accidentally swallowed during instillation, Avamis is not absorbed into the bloodstream and does not have a systemic effect. The drug has a number of advantages in comparison with other nasal hormones and, first of all, this is due to the good tolerance of the drug and the absence of serious contraindications to its appointment. Only the appointment of Avamis to people with severe violations of the functional ability of the liver requires caution. The use of the drug for pregnant and lactating women is not recommended due to the insufficient number of studies on its effect. Children are prescribed Avaris from the age of two. Cases of overdose with this drug were also not recorded. Polydexa
The drug is significantly different from all previous ones. This is a combined drug that includes drugs of three groups, namely antibiotics (neomycin and polymyxin sulfate), vasoconstrictors (phenylephrine hydrochloride) and hormones (dexamethasone 0.25 mg). Due to the presence of an antibiotic, Polydex is active against bacterial infections (the only exceptions are representatives of the cocci group). Therefore, its appointment is justified for persons with diseases of the nasopharynx of an allergic nature, in the presence of an infectious agent. Polydex is made in the form of drops and spray. Drops, as a rule, are used only in the treatment of inflammatory diseases of the ear, however, their use for the treatment of inflammatory processes in the nose is also permissible. Drops are released in yellow-brown bottles with a capacity of 10.5 ml. The spray, unlike ear drops, includes phenylephrine in its composition and is available in a blue bottle (15 ml), protected from daylight. The duration of drug therapy is on average 5-10 days, with prolonged use of the drug, the risk of developing candidiasis and nasopharyngeal dysbiosis is high. The use of Polydex is absolutely contraindicated in viral diseases of the nasopharynx, angle-closure glaucoma, severe renal dysfunction, as well as during pregnancy and breastfeeding. The drug is not prescribed for children under two years of age. It is forbidden to simultaneously use Polydex with antibacterial aminoglycoside drugs. Comparative characteristics of nasal corticosteroids
Given the variety of nasal hormonal drugs, it is often difficult for a person to distinguish between them by action and give preference to any of them. Below is a table, the main purpose of which is to simplify the understanding of the main differences between nasal corticosteroids.  Despite the fact that hormonal drugs in the form of nasal sprays do not enter the general circulation, the risk of adverse reactions remains high. With this in mind, the choice of corticosteroids should be taken very seriously.
In the treatment of a number of diseases of the musculoskeletal system, especially of an inflammatory nature, drugs such as glucocorticosteroids have found widespread use. Before you understand the main therapeutic effects, indications and contraindications, you need to know what glucocorticosteroids (GCS) are. Glucocorticosteroids are drugs belonging to the group of steroid hormones and possessing anti-inflammatory, antiallergic, anti-shock, immunosuppressive and other properties. Classification
Today, there are several classifications of glucocorticosteroids according to various parameters. The most clinically significant classification is considered, which separates drugs according to the duration of their action. According to her, the following drug groups are distinguished:
When is it used?In the treatment of diseases of the joints and the spine, the main indication for the use of glucocorticosteroids is considered to be a severe inflammatory process, which is particularly intense and does not lend itself to therapy with non-steroidal anti-inflammatory drugs. Which articular pathologies can be used for:
When prescribing GCS, the doctor tries to achieve the maximum therapeutic effect using the minimum dosage of the drug. The regimen of glucocorticosteroid treatment depends more on the severity of the disease, the patient's condition and his response to therapy, than on age and weight. Clinical efficacySeveral recent scientific studies have shown the high effectiveness of the use of glucocorticosteroids in the treatment of severe forms of joint inflammation. A quick clinical effect is also possible to achieve with the simultaneous use of corticosteroids in low doses and non-steroidal anti-inflammatory drugs. It was found that most patients with disabilities due to polyarthritis become much easier in functional terms after several days of GCS therapy. What the doctor expects when prescribing glucocorticosteroids:
Clinical experience has shown that many patients with rheumatoid arthritis often become functionally dependent on glucocorticosteroid therapy and are forced to switch to long courses of their use, which undoubtedly leads to the development of side effects. How is it used?
Several routes of administration of GCS preparations are possible. As a rule, in the treatment of inflammatory pathology of the musculoskeletal system, glucocorticosteroids are injected into the joint. By directly acting on the site of inflammation, the maximum therapeutic effect is achieved. It should be noted that quite often liquid (exudate) can accumulate in the cavity of large joints. In such cases, it is first necessary to remove this fluid, and only then to carry out intra-articular administration of the drug. Sometimes, in order to achieve a better effect, the administration of GCS inside the joint is combined with glucocorticosteroid therapy in tablets. This type of treatment is used for severe forms of the inflammatory process with a pronounced tendency to progression.
GCS preparations are also quite often prescribed orally in the form of tablets or injected parenterally (into a vein or muscle). the duration of the course and the dosage of the medication depend on the severity and nature of the disease. For some patients, the therapeutic course is several months or even years. With a high activity of the pathological process in the joints, the so-called pulse therapy is used. In this case, the drug is administered intravenously (through a dropper) for 3 consecutive days. In most cases, pulse glucocorticosteroid therapy can quickly suppress the activity of the inflammatory process. Contraindications
GCS drugs, like many other drugs, may not be prescribed to all patients. Depending on the route of administration of the drug, certain contraindications must be taken into account. For example, intravenous, intramuscular or oral glucocorticosteroids should not be used for the following diseases or pathological conditions:
In addition, GCS is not injected into the affected joint for increased bleeding, severe osteoporosis, and ineffectiveness from previous injections. Also, this route of administration for glucocorticosteroids is contraindicated in intra-articular fractures, periarthritis of an infectious nature and before joint surgery (arthroplasty).
Adverse reactions
According to clinical observation, despite the fact that most of the side effects from long-term use of GCS in inflammatory diseases of the joints and spine are considered quite severe, some of them appear an order of magnitude less often than with other anti-inflammatory drugs. Many experts conditionally divide the side effects with prolonged systemic use of glucocorticosteroids into two groups:
At the same time, it was found that the use of non-steroidal anti-inflammatory drugs more often provokes the development of severe erosive and ulcerative pathology of the gastrointestinal tract than the use of drugs from the GCS group. Treatment with glucocorticoids is justifiably associated with an increased risk of infectious complications, but this is typical mainly for patients who receive high doses of drugs. Mention should be made of the criteria for inadequate glucocorticosteroid therapy:
With intra-articular administration of corticosteroids, one of the most dangerous, but rather rare complications, is infection in the articular cavity during the injection. In addition, the immunosuppressive property of glucocorticoids contributes to the development of a purulent inflammatory process. In rare cases, "post-injection synovitis" can be observed, when after the injection there is an increase in the inflammatory process in the synovial membrane of the joint, which can last from several hours to 2-3 days. It is highly undesirable to inject the drug into muscle tissue, since atrophic or necrotic processes may develop. Glucocorticosteroid osteoporosis One of the most unfavorable complications of long-term glucocorticosteroid treatment is. Nevertheless, according to some experts, the high inflammatory activity of rheumatoid arthritis and a decrease in physical activity are considered no less important factors in the onset of osteoporosis than long-term treatment with GCS. To reduce the risk of developing this complication, many doctors recommend significantly adjusting their lifestyle, especially for those patients who receive glucocorticosteroids for a long time. What exactly needs to be done:
Pregnancy and lactationNo targeted clinical trials have been conducted on the safety of glucocorticosteroid use during pregnancy. However, doctors may prescribe this drug to a pregnant woman, but only if the expected effect of the treatment significantly outweighs the perceived risk to the child. In addition, breastfeeding mothers are strongly advised to suspend breastfeeding during glucocorticosteroid therapy. Overdose
When an overdose of GCS drugs occurs, a significant increase in blood pressure, edema of the lower extremities, and increased side effects of the drug itself can be observed. If an acute overdose is recorded, then it is necessary to rinse the stomach as soon as possible or provoke vomiting. If the condition worsens, you should immediately contact a specialized medical institution. A specific antidote has not yet been developed. InteractionMultiple scientific studies have proven that glucocorticosteroids interact with many drugs, provoking the development of various adverse reactions. In order to avoid the appearance of undesirable effects, it is recommended to consult with your doctor before combining the use of GCS with any other medicine. Price
To buy any drug from the glucocorticosteroid group, you must have a prescription. It will not be superfluous to remind once again that all GCS have very specific application features and a very wide range of adverse reactions, therefore, self-medication is strongly discouraged. For informational purposes only, we give the prices for some medicines:
The site provides background information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. A specialist consultation is required! General informationGlucocorticoids called steroid hormones secreted by the adrenal cortex, as well as their artificial analogs used in medicine.The first samples of these drugs date back to the 40s of the twentieth century and the first hormones used were hydrocortisone and cortisone. In total, to date, five hormones of this group have been studied ( are presented by the degree of impact on processes in the body, decreasing):
Classification of drugsAll drugs in this group are divided into:
According to the duration of exposure, all drugs can be divided into:
ActScientists have not yet fully figured out the mechanism of action of these hormones on the body. Getting into the cell through the cell membrane, the hormone acts on receptors that are sensitive to steroid substances, is sent together with the receptor to the cell nucleus and participates in the production of special protein components involved in the inflammatory process.Hormones affect the following processes in the body:
Indications
ContraindicationsAbsolute:
If we are talking about urgent saving the patient's life, drugs are used in any case. Learn more about essential drugs Cortisone CortisoneIt is used for replacement therapy in patients with adrenal insufficiency. Produced in tablets. Used only in normal liver function. Affects the exchange of water and salts. Hydrocortisone It is prescribed for adrenal insufficiency. Not recommended for edema, heart failure, hypertension, as it promotes sodium retention in the body and potassium excretion. It is produced in the form of a liquid for injection, suspension. Prednisolone Methylprednisolone Dexamethasone Betamethasone Preparations in the form of inhalationBeclomethasone - the drug is used in the treatment of bronchial asthma, relieves inflammation and relieves allergies. When used in the form of inhalation, it is practically not absorbed into the blood and does not act systemically.Contraindications:
Budesonide - the main therapy of bronchial asthma, chronic obstructive pulmonary disease. pregnancy, breastfeeding, fungal, viral and bacterial diseases of the respiratory system, tuberculosis. The drug can provoke a coughing attack, dry mouth, migraine-like pain, stomatitis, nausea, hyperactivity. Fluticasone - the drug is prescribed for bronchial asthma and chronic obstructive pulmonary disease as the main remedy.
This medication is not used to relieve asthma attacks. Preparations for systemic use For systemic use, drugs have been created prednisone, cortisone. For systemic use, drugs have been created prednisone, cortisone.There are many drugs that are used both locally and systemically. These include: betamethasone, dexamethasone, triamcinolone, fludrocortisone, mazipredone, methylprednisolone, prednisolone. Such drugs are used both in the form of tablets for oral use and in injection. Ointments, creams, lotionsGlucocorticoids for external use are available in the form of ointments, gels, creams, lotions. They are prescribed for some dermatological diseases of a non-infectious nature.Indications:
How to choose the right dosage form of the drug?
Creams can cause irritation or dryness if the skin has wounds. They are prescribed for intertriginous phenomena. This form does not leave greasy stains and is quickly absorbed. Lotions are indicated for weeping phenomena, very convenient for treating the scalp. All glucocorticosteroids used in dermatology are divided into four groups according to their potency:
Side effectsGlucocorticosteroid drugs really quickly relieve many of the unwanted symptoms of diseases. However, they cause a lot of side effects. Therefore, they are prescribed only in those cases when no others are already able to help.Especially many side effects are observed with the systemic use of these drugs. Several new methods of using these drugs have been developed, which slightly reduce the likelihood of unwanted effects. But treatment with these drugs in any case requires constant monitoring of the patient's overall health. When using steroid hormonal drugs, the following side effects are likely to develop:
Application during pregnancy Despite the fact that these drugs easily penetrate the placental barrier, they do not cause severe disturbances in fetal formation. It is safer to consume natural or non-fluorinated products during pregnancy. Fluoridated ones, if consumed long enough, can provoke fetal development disorders. Despite the fact that these drugs easily penetrate the placental barrier, they do not cause severe disturbances in fetal formation. It is safer to consume natural or non-fluorinated products during pregnancy. Fluoridated ones, if consumed long enough, can provoke fetal development disorders. In some cases, drugs of the glucocorticoid group are even specially prescribed when there is a likelihood of miscarriage to maintain pregnancy. Although, the use of such drugs is usually made only for health reasons, which include:
During lactation, the use of low dosages of steroid drugs ( in terms of not exceeding 5 mg prednisolone) can not harm the baby, because glucocorticoids enter breast milk in small doses. If the course of treatment is long, and the dosages are high, the child may experience inhibition of growth and development, as well as suppression of the adrenal glands, hypothalamus and pituitary gland. |
| Read: |
|---|
New
- Beach hairstyles for different hair lengths
- Epic nicknames. The best nicknames for games. For girls in English
- Image of learning activity
- How limestone turns into marble
- Promising methodology "school of animals"
- Games about primitive people on pc
- Cathedrals of Kiev Cathedral of the Assumption of the Blessed Virgin
- What the year will be dedicated to
- Prince yaroslav the wise. Prince Yaroslav the Wise. Yaroslav the Wise - Monument "1000th Anniversary of Russia"
- File extension CAP Extension cap